-
PDF
- Split View
-
Views
-
Cite
Cite
Feng-Jen Tsai, Howard Lee, Victoria Y. Fan, Perspective and investments in health system strengthening of Gavi, the Vaccine Alliance: a content analysis of health system strengthening-specific funding, International Health, Volume 8, Issue 4, July 2016, Pages 246–252, https://doi.org/10.1093/inthealth/ihv063
Close - Share Icon Share
Abstract
This paper aimed to compare the health systems strengthening (HSS) framework of Gavi and WHO and to analyze resource allocation in HSS by Gavi.
Among 76 countries which received HSS funding from Gavi from 2006 to 2013, summary reports of 44 countries and approved proposals of 10 countries were collected. After comparing the HSS framework of WHO and Gavi, each activity described in documents was categorized according to Gavi's framework and funding allocation was analyzed.
Compared with WHO's HSS framework, Gavi's has a distinctive function within the building block ‘Drugs, Equipment, Supplies, Facilities’ and a distinctive function of ‘providing incentive and bonuses’ under the building block ‘Human Resource/Performance Management’. Gavi has steadily invested 10% of their total budget on HSS, but 47% were allocated in these categories, whereas 78% were for activities arguably not covered by WHO's HSS framework. In Africa, 70% of Gavi's budget fell under ‘Drugs, Equipment, Supplies, Facilities’ and 92.8% were for activities arguably not deemed as HSS by WHO.
Gavi's HSS support emphasized inputs with short-term measurable outcomes. Harmonization of the concept of HSS and collaboration between Gavi and multilateral international agencies, such as World Bank and WHO, are needed.
Introduction
In the last two decades, global health initiatives (GHIs) such as the Global Fund Against AIDS, Tuberculosis, and Malaria, and the Gavi, the Vaccine Alliance, have targeted specific diseases or conditions, in part to meet the Millennium Development Goals (MDGs).1 However, this vertical approach has been shown in some cases to negatively affect national health systems.2–5 The emergence of global attention to health systems strengthening (HSS) in the late 2000s was in part a response to such findings.6,7
In 2007, WHO promoted a framework for HSS detailing six ‘building blocks’ describing the different public health functions (Service Delivery, Health Workforce, Information, Medical Products, Vaccines And Technologies, Sustainable Financing and Social Protection, and Leadership/Governance).8 Many other global-health actors, including the Global Fund and Gavi, incorporated the concept ‘HSS’ into their mandates and started to invest in it.4,9–11 However, questions have been raised regarding the definitions and theoretical frameworks of HSS and doubts as to whether investments in HSS by GHIs are in fact effective towards strengthening health systems or if HSS is being used as a pass-through or container concept for selective, disease-specific interventions.12–16 Despite past research focusing on conceptual perspectives and theories and the search to find a solution for harmonizing various analytical frameworks of health systems, studies on analyzing cash flows of global-health initiatives have mainly focused on a single or particular dimension of a health system such as the health workforce, without necessarily revealing and analyzing the initiative's particular logic or approach towards health systems.17–21 Given the significant financial resources for health controlled by GHIs and their assumed dominant positions within global health policy networks, it is important to better understand a GHI's perspective towards HSS.22,23 In addition, although there are extensive literature on disease-specific investments by GHIs and their impact, studies on HSS-specific funding are relatively rare.24,25 Therefore, this paper aims to understand the concept of HSS of one important GHI, Gavi, by analyzing their HSS-specific funding allocations.
Gavi was formed in 1999 with the aim of influencing market mechanisms for vaccine development and procurement. As a global-health agency with a vertical approach on the provision of vaccines, Gavi began to fund HSS from 2005.26,27 Today, Gavi calls ‘HSS support’ a ‘key principle of Gavi's mission’ and a ‘health system goal’ is among its strategic objectives. With the intention to strengthen health systems to ‘scale-up new vaccines and to improve immunisation coverage and equity’, Gavi has already invested US$568 million to HSS in 53 different countries by the end of 2010 and has continued to fund its HSS programs.28 Although Gavi has adopted HSS as its key principle, Storeng interviewed related key persons of Gavi and found that Gavi's HSS support has become emblematic of the so-called ‘Gates approach’, i.e., focused on targeted technical solutions with clear, measurable outcomes, which can run counter to the concept of HSS that emphasizes multiple social and political dimensions.29 This apparent paradox of Gavi raises questions about the content of Gavi's HSS. How much of Gavi's HSS-labeled funding is actually invested in activities that could be deemed as HSS activities? Perhaps more importantly, what is the logic underpinning Gavi's HSS?
This paper intends to understand Gavi's perspective and investments in HSS, specifically by looking at its resource allocation in each of the HSS building blocks as well as comparing the Gavi HSS framework to the WHO HSS framework. While WHO's HSS framework is defined in terms of essential functions of a health system (a relatively widely used framework), we used the WHO framework in this study to classify Gavi-funded activities by WHO building block.
Methods
In order to understand the historical allocation of budget on HSS by Gavi, we first collected information regarding Gavi's commitments and disbursements for funding from Gavi's website. Next, information regarding Gavi's approval for funding was used for analysis.
Documents of all the countries that had their HSS proposals approved from 2006 to 2013 were collected for content analysis. HSS summary reports were downloaded from the Gavi website on 7 November 2013. The reports included information such as date of approval, total budget approved by the board, total amount of disbursement to date, last disbursement date, national health policy goals, proposal goals, as well as a breakdown of the budget according to the six main categories of HSS. For countries without summary reports, the approved HSS proposals were downloaded from the Gavi website on 10 December 2013. The proposals included the application development process, country background information, situation analysis/needs assessment, goals and objectives of Gavi HSS support, Gavi HSS activities and implementation schedule, objectives, monitoring and evaluation, implementation arrangements, cost and funding for Gavi HSS, and endorsement of the application. From 2006 to 2013, 76 countries received some funding from Gavi. Of these 76 countries, 14 did not receive funding for HSS, 4 did not have an HSS summary or proposal available, and 4 did not provide sufficiently detailed information regarding budgets. Thus, a total of 54 countries were included and analyzed in our study. Of these 54 countries, 44 countries had health summaries and 10 had only proposals.
We used the framework that Gavi used within their HSS summaries as Gavi's HSS framework to analyze funding allocations. To understand the compatibility between the framework used by Gavi and the framework proposed by WHO, we compared these two frameworks first. All the functions under each major building block were identified and matched with WHO's Framework for Action. For example, ‘financial management’ is a function under ‘Governance, Management, Organization’ in the Gavi HSS framework, which we matched to the WHO HSS priority in the ‘sustainable financing and social protection’ building block.
Then each HSS activity described in the countries' documents under Gavi's building block or functions that were not in-line with WHO's HSS framework were categorized in accordance with the framework by two coders. Before coding, coders read the documents and discussed the standard for classification. Based on the consensus, activity was categorized and between-coder agreement was 92%. Descriptive analysis was then conducted by Microsoft Excel (Microsoft Corp., Redmond, WA, USA).
Results
Historical funding allocation on health systems strengthening by Gavi from 2007 to 2015
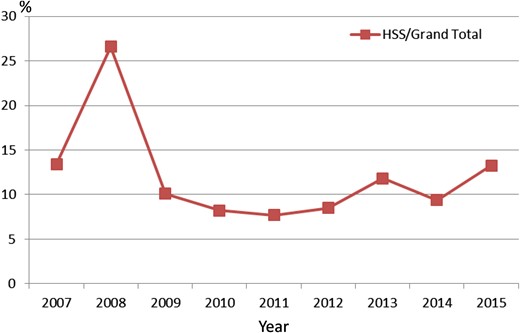
The yearly percentage of HSS budget allocated by Gavi is shown in Figure 1. The first HSS project was approved by Gavi in 2007. In 2008, the funding on HSS reached 27% of Gavi's total budget. Although Gavi placed less than 10% funding on HSS between 2009 and 2012, the percentage increased again from 2013. The total budget on HSS from Gavi was US$955 981 434. By year, the lowest amount of HSS funding was in 2010 with US$38 822 850, and the highest amount was in 2015 with US$178 128 670.
Historical budget allocation on health systems strengthening by GAVI, 2007–2015. This figure is available in black and white in print and in color at International Health online.
Health systems strengthening framework comparison between WHO and Gavi
There are six main building blocks for the Gavi framework: Governance, Management, Organizational; Human Resources/Performance Management; Drugs, Equipment, Supplies, Facilities; Monitoring and Evaluation; Operational Research; and Support Costs. It also combines the three themes identified to guide applicant countries: 1. Health workforce mobilization, distribution and motivation at district level and below. 2. Drugs, equipment and infrastructure supply, distribution and maintenance. 3. Organization, monitoring and management of health services at district levels and below. Detailed functions of each building block are shown in Table 1. The six WHO building blocks are: Service Delivery; Health Workforce; Information; Medical Products, Vaccines and Technologies; Sustainable Financing and Social Protection; and Leadership/Governance. The specific priorities of each WHO building blocks were matched with the function and building blocks of Gavi's HSS framework and shown in Table 1.
WHO and Gavi health systems strengthening framework comparison
| Gavi Framework for HSS . | WHO Framework for HSS . | ||
|---|---|---|---|
| Building block . | Functions . | Building block . | Priorities . |
| Governance, Management, Organizational | Policy making, establishment of regulations | Governance/ Leadership | Policy guidance, regulation design |
| Financial management | Sustainable Financing and Social Protection | Raising funds and reducing out of pocket payments | |
| Logistical management | Service Delivery | Organisation of the provider network | |
| Cohesion of health system | Governance/Leadership | System design | |
| Coordination between government, partners and stakeholders | Governance/Leadership | Collaboration and coalition building | |
| Human Resources/ Performance Management | Human resource management system | Health Workforce | Adequate regulatory mechanism for human resources |
| Decrease staffing shortage | Health Workforce | Retain effective workforce | |
| Training qualified personnel | Health Workforce | Design training programmes, financing education | |
| Providing incentives and bonusesa | NA | NA | |
| Community engagement | Health Workforce | Engagement of stakeholders and partners | |
| Drugs, Equipment, Supplies, Facilitiesb | Construction, refurbishment and maintenance of health facilities | NA | NA |
| Provide transportation | NA | NA | |
| Provide drugs and vaccines | NA | NA | |
| Monitoring and Evaluation | Development of health information system | Information | Capacity to synthesize information and promote application of knowledge |
| Development of supervisory tools | Information | Capacity to detect and investigate | |
| Develop communication infrastructure | Information | Capacity to communicate | |
| Epidemiological surveillance and monitoring | Information | Generate data | |
| Operational Research | Systems research | Information | Generate intelligence and research |
| Support Costs | Administrative costs etc. | NA | NA |
| Gavi Framework for HSS . | WHO Framework for HSS . | ||
|---|---|---|---|
| Building block . | Functions . | Building block . | Priorities . |
| Governance, Management, Organizational | Policy making, establishment of regulations | Governance/ Leadership | Policy guidance, regulation design |
| Financial management | Sustainable Financing and Social Protection | Raising funds and reducing out of pocket payments | |
| Logistical management | Service Delivery | Organisation of the provider network | |
| Cohesion of health system | Governance/Leadership | System design | |
| Coordination between government, partners and stakeholders | Governance/Leadership | Collaboration and coalition building | |
| Human Resources/ Performance Management | Human resource management system | Health Workforce | Adequate regulatory mechanism for human resources |
| Decrease staffing shortage | Health Workforce | Retain effective workforce | |
| Training qualified personnel | Health Workforce | Design training programmes, financing education | |
| Providing incentives and bonusesa | NA | NA | |
| Community engagement | Health Workforce | Engagement of stakeholders and partners | |
| Drugs, Equipment, Supplies, Facilitiesb | Construction, refurbishment and maintenance of health facilities | NA | NA |
| Provide transportation | NA | NA | |
| Provide drugs and vaccines | NA | NA | |
| Monitoring and Evaluation | Development of health information system | Information | Capacity to synthesize information and promote application of knowledge |
| Development of supervisory tools | Information | Capacity to detect and investigate | |
| Develop communication infrastructure | Information | Capacity to communicate | |
| Epidemiological surveillance and monitoring | Information | Generate data | |
| Operational Research | Systems research | Information | Generate intelligence and research |
| Support Costs | Administrative costs etc. | NA | NA |
HSS: health systems strengthening; NA: not applicable.
a Providing bonuses do not necessarily develop a sustainable incentive system (part of the WHO building block Health Workforce).
b Developing good manufacturing practices, procurement systems and guidelines for efficient use of resources count as health systems strengthening, whereas the mere purchasing of items do not.
WHO and Gavi health systems strengthening framework comparison
| Gavi Framework for HSS . | WHO Framework for HSS . | ||
|---|---|---|---|
| Building block . | Functions . | Building block . | Priorities . |
| Governance, Management, Organizational | Policy making, establishment of regulations | Governance/ Leadership | Policy guidance, regulation design |
| Financial management | Sustainable Financing and Social Protection | Raising funds and reducing out of pocket payments | |
| Logistical management | Service Delivery | Organisation of the provider network | |
| Cohesion of health system | Governance/Leadership | System design | |
| Coordination between government, partners and stakeholders | Governance/Leadership | Collaboration and coalition building | |
| Human Resources/ Performance Management | Human resource management system | Health Workforce | Adequate regulatory mechanism for human resources |
| Decrease staffing shortage | Health Workforce | Retain effective workforce | |
| Training qualified personnel | Health Workforce | Design training programmes, financing education | |
| Providing incentives and bonusesa | NA | NA | |
| Community engagement | Health Workforce | Engagement of stakeholders and partners | |
| Drugs, Equipment, Supplies, Facilitiesb | Construction, refurbishment and maintenance of health facilities | NA | NA |
| Provide transportation | NA | NA | |
| Provide drugs and vaccines | NA | NA | |
| Monitoring and Evaluation | Development of health information system | Information | Capacity to synthesize information and promote application of knowledge |
| Development of supervisory tools | Information | Capacity to detect and investigate | |
| Develop communication infrastructure | Information | Capacity to communicate | |
| Epidemiological surveillance and monitoring | Information | Generate data | |
| Operational Research | Systems research | Information | Generate intelligence and research |
| Support Costs | Administrative costs etc. | NA | NA |
| Gavi Framework for HSS . | WHO Framework for HSS . | ||
|---|---|---|---|
| Building block . | Functions . | Building block . | Priorities . |
| Governance, Management, Organizational | Policy making, establishment of regulations | Governance/ Leadership | Policy guidance, regulation design |
| Financial management | Sustainable Financing and Social Protection | Raising funds and reducing out of pocket payments | |
| Logistical management | Service Delivery | Organisation of the provider network | |
| Cohesion of health system | Governance/Leadership | System design | |
| Coordination between government, partners and stakeholders | Governance/Leadership | Collaboration and coalition building | |
| Human Resources/ Performance Management | Human resource management system | Health Workforce | Adequate regulatory mechanism for human resources |
| Decrease staffing shortage | Health Workforce | Retain effective workforce | |
| Training qualified personnel | Health Workforce | Design training programmes, financing education | |
| Providing incentives and bonusesa | NA | NA | |
| Community engagement | Health Workforce | Engagement of stakeholders and partners | |
| Drugs, Equipment, Supplies, Facilitiesb | Construction, refurbishment and maintenance of health facilities | NA | NA |
| Provide transportation | NA | NA | |
| Provide drugs and vaccines | NA | NA | |
| Monitoring and Evaluation | Development of health information system | Information | Capacity to synthesize information and promote application of knowledge |
| Development of supervisory tools | Information | Capacity to detect and investigate | |
| Develop communication infrastructure | Information | Capacity to communicate | |
| Epidemiological surveillance and monitoring | Information | Generate data | |
| Operational Research | Systems research | Information | Generate intelligence and research |
| Support Costs | Administrative costs etc. | NA | NA |
HSS: health systems strengthening; NA: not applicable.
a Providing bonuses do not necessarily develop a sustainable incentive system (part of the WHO building block Health Workforce).
b Developing good manufacturing practices, procurement systems and guidelines for efficient use of resources count as health systems strengthening, whereas the mere purchasing of items do not.
For the most part, Gavi's building block of Governance, Management and Organizational matched with the WHO's building block of Governance/Leadership. Gavi's building block of Human Resources/Performance Management matched with WHO's building block of Health Workforce. Additionally, Gavi's building block of Operational Research and Monitoring and Evaluation matched with WHO's building block of Information. Also, there are functions within Gavi's HSS building blocks that do not exactly match with the corresponding WHO block but are nevertheless encompassed under a different building block in the WHO framework. For example, the function of ‘financial management’ in Gavi's building block of Governance, Management, Organizational arguably matched more with WHO's building block of Sustainable Financing and Social Protection than the building block of Governance/Leadership.
However, there were two parts of the Gavi's framework that appeared incompatible with the WHO framework on strengthening of health systems; namely, the Gavi building block ‘Drugs, Equipment, Supplies, Facilities’ and the other being the function of providing incentive and bonuses under Human Resource/Performance Management. A significant part of Gavi HSS funding goes toward procuring drugs, equipment, supplies and refurbishing or maintaining facilities such as purchasing fly traps, albendazole and praziquantel for Malawi, providing essential medicines and medical products to hospitals and health clinic in Chad, purchasing vaccines, materials for injection and logistics in Burundi, purchasing and distributing motorcycles in Cuba, or purchasing fuel for ambulances and hospital generators for Sierra Leone. Such funding, though categorized as HSS under Gavi, does not fit into the WHO framework for HSS because under the WHO framework, purchasing goods is equivalent to donating resources and such short-term solutions do little for the long-term development of the healthcare system. While such activities might be conceived as affecting the health system, they do not necessarily ‘strengthen’ the system. Similarly, part of the Gavi HSS funding went to providing bonuses for health personnel such as payment of performance bonuses in Central African Republic and reinforcing motivation system by financial incentive bonuses in Mali. Such direct financial payment as incentives for health workers does not count as HSS under the WHO framework that requires the development of a sustainable financing system rather than the use of ad hoc payments.
Gavi health systems strengthening funding allocation from 2006 to 2013
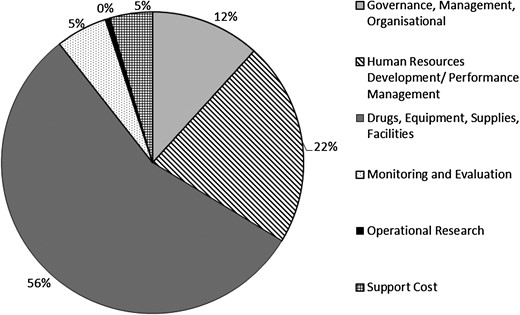
HSS funding allocation by Gavi from 2006 to 2013 are shown in Figure 2. Among total HSS funding, the category of Drugs, Equipment, Supplies, Facilities accounted for 56% of HSS funding. This was followed by the Human Resources/Performance Management category at 22%. Operational Research received less than 1% funding. In terms of regional allocations, Africa received over half of the HSS funding at 53%, followed by Asia at 46%. South and Central America accounted for 1% and Europe received less than 1% of HSS funding.
Distribution of GAVI health systems strengthening funding by health systems category, 2006–13. HSS: health systems strengthening.
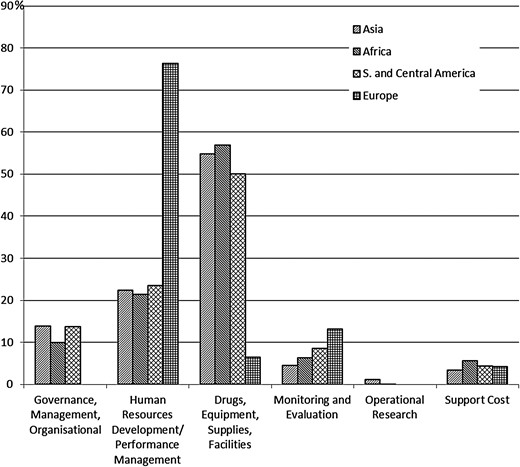
Most regions with the exception of Europe had a similar distribution of HSS funds across the Gavi HSS categories (Figure 3). In Asia, Africa and South and Central America, 55% of the funding went to Drugs, Equipment, Supplies, Facilities. Human Resources/Performance Management took up 22% of the funding while Governance, Management, Organizational received 14%. In Europe, unlike the other regions, most of the HSS funding was allocated to Human Resources/Performance Management (76%). Operational Research was negligible in all of the continents.
Percentage of funding allocated to each health systems strengthening building block by continent, 2006–2013.
Analysis of Gavi health systems strengthening investments not compatible with the WHO framework from 2006 to 2013
According to our previous analysis, Gavi's funding in Drugs, Equipment, Supplies, Facilities and in providing bonuses for health workers in the building block of Human Resources/Performance Management were incompatible with WHO's HSS framework. Further analysis of detailed information regarding the activities described in each block showed that 47.4% of total HSS Gavi investment were in these two categories and, hence, were not compatible with the HSS framework set out by WHO. Of these two Gavi building blocks, Drugs, Equipment, Supplies, Facilities had the higher proportion of incompatible funding at 78.7%, whereas only 15.8% of funding in Human Resources/Performance Management was incompatible (i.e., due to the use of bonuses).
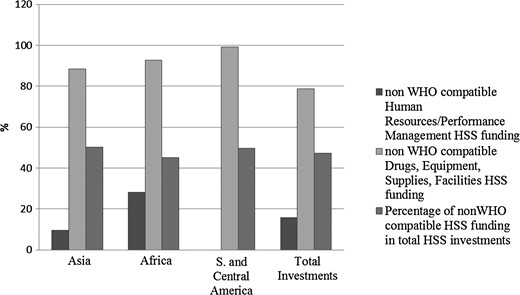
The proportion of funding for Drugs, Equipment, Supplies, Facilities that was incompatible is higher in priority regions: 92.8% in Africa; 88.3% in Asia; and 99.2% in South and Central America. In terms of the compatibility to the WHO framework of the funding for Human Resources/Performance Management, 28% of funding was incompatible in Africa, 9.6% in Asia, and, notably, none in South and Central America. The percentage of Gavi HSS funding that we deemed incompatible with the WHO HSS framework by region is presented in Figure 4.
Percentage of GAVI Health Systems Strengthening funding deemed not compatible by region, 2006–2013.
Discussion
This study analyzes the HSS spending by countries and region funded by Gavi after Gavi's support for HSS funding since 2007. While Gavi's HSS framework was basically compatible with WHO's HSS framework, Gavi has distinctive functions within its building block ‘Drugs, Equipment, Supplies, Facilities’ and building block ‘Human Resource/Performance Management’. This study also showed that, although Gavi steadily invested around 10% of their total budget on HSS, almost half of the budget was allocated in categories that were not covered by the WHO HSS framework.12,30 The challenge of such funding by Gavi is that it provided short-term funds for things (medicines, supplies, facility maintenance) as well as people (top-up payments). Although HSS defined by WHO's framework has some weakness, most studies focusing on HSS have shared the consensus that expenditures on medicines and other consumables are not strengthening health systems even though they may be supporting health systems, due to the short-term effects on health systems.18 Such activities are not long-term solutions that strengthen the system to becoming a sustainable health system, but rather are supporting the health system in the short term.12,30 Thus, whereas the concept of HSS can arguably focus on the root causes of health system weaknesses through a holistic and integrated approach, Gavi's HSS strategies have continued to emphasise ‘rapid-impact interventions’ and measurable short-term outcomes. Other studies of other GHI funding for HSS reported similar findings, e.g., that the Global Fund dedicated resources on selective operational interventions without system-level support due to its ‘diagonal’ approach to HSS.17 Although these investments not in-line with WHO's HSS framework also supported the health system, the contribution of these funding on strengthening the health system might be limited.
Furthermore, there is a need for allocation adjustment in several of the continents, especially in Africa. Specifically, 70% of budget allocated to Africa for HSS activities fall under Drugs, Equipment, Supplies, Facilities and almost all of them were invested in activities that supported the health system but were not covered in WHO's HSS framework. Although availability and affordability of essential medicines remained inadequate in African countries, investing in medicines without focusing on other systemic factors like irrational use of available resources, lack of national drug and vaccine policies, or lack of institutions to develop those policies such as national advisory committees on immunization might not be helpful in strengthening the health system in recipient countries.31 With the continued absolute growth of global health development assistance aid for specific diseases, recipient countries are not necessarily supported to strengthen their health system.32 This study has identified the gap between what is labeled as ‘health systems strengthening’ versus what would help to strengthen the health system in the long run. We noted that a fifth of the budget allocated to Africa for HSS falls under Human Resources/Performance Management and 28% of it were for activities not covered in WHO's HSS framework. Several organizations such as Gavi and the World Bank are committed to using performance-based incentives as a means to achieve short-term outcomes, but raises longer term questions of the efficiency and sustainability of such approaches.33
There are limitations to this study. First, while recipient countries might change the proposed activities during implementation, the 10 proposals out of 54 HSS grants analyzed in our study might not represent the actual allocation of funds. Second, the resource allocation might be biased due to the unavailability of detailed activity-wise itemization of funding and subjectivity in grant categorization. Third, we might overestimate Gavi's funding in HSS defined by WHO framework due to the assumption that the activity categorized in the building block or functions which in-line with WHO's HSS framework was indeed HSS activities. Finally, reasonable people could disagree about whether short-term funds for performance bonuses and drug purchases strengthen or only support the health system.
Conclusions
In conclusion, this study found a lack of complete convergence between Gavi's and WHO's HSS framework that pointing to ambiguities in the definition and understanding of what constitutes HSS. While the study result showed that the bulk of Gavi's HSS funding is focused on overcoming input shortage and fulfilling short-term result-oriented objectives rather than reforming or redesigning health systems, investments in systemic reforms are nevertheless required for GHIs to achieve their disease-specific goals. Although differential allocations across continents might in fact reflect region-specific requirements for HSS funding, more allocation adjustments are needed in order to effectively strengthen the health system of the region. While GHIs like Gavi may have a disease-specific mandate and focused capacities, others like WHO and the World Bank might be better able to tackle sector-wide reforms. A harmonized strategy towards HSS is, therefore, essential. Recent initiatives like the International Health Partnership Plus (IHP+) are a step in the right direction, but further movement of the network and widespread adoption of that platform as a substitute for siloed approaches is crucial for the development of HSS.
Authors' contributions: FJT carried out the design of the study, interpreted the data and drafted the manuscript. HL participated in collecting the data, interpreting the data and helped to draft the manuscript. VF contributed to the writing of the manuscript. All authors read and approved the final manuscript. FJT is guarantor of the paper.
Funding: This study received partial funding from the National Science Council of Taiwan (now named as Ministry of Science and Technology). Project number: NSC102-2815-C-038-078-B.
Competing interests: None declared.
Ethical approval: Not required.



Comments