-
PDF
- Split View
-
Views
-
Cite
Cite
Edwine W Barasa, Keith Cloete, Lucy Gilson, From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening, Health Policy and Planning, Volume 32, Issue suppl_3, November 2017, Pages iii91–iii94, https://doi.org/10.1093/heapol/czx118
Close - Share Icon Share
Abstract
Recent health system shocks such as the Ebola disease outbreak have focused global health attention on the notion of resilient health systems. In this commentary, we reflect on the current framing of the concept of resilience in health systems discourse and propose a reframing. Specifically, we propose that: (1) in addition to sudden shocks, health systems face the ongoing strain of multiple factors. Health systems need the capacity to continue to deliver services of good quality and respond effectively to wider health challenges. We call this capacity everyday resilience; (2) health system resilience entails more than bouncing back from shock. In complex adaptive systems (CAS), resilience emerges from a combination of absorptive, adaptive and transformative strategies; (3) nurturing the resilience of health systems requires understanding health systems as comprising not only hardware elements (such as finances and infrastructure), but also software elements (such as leadership capacity, power relations, values and appropriate organizational culture). We also reflect on current criticisms of the concept of resilient health systems, such as that it assumes that systems are apolitical, ignoring actor agency, promoting inaction, and requiring that we accept and embrace vulnerability, rather than strive for stronger and more responsive systems. We observe that these criticisms are warranted to the extent that they refer to notions of resilience that are mismatched with the reality of health systems as CAS. We argue that the observed weaknesses of resilience thinking can be addressed by reframing and applying a resilience lens that is better suited to the attributes of health systems as CAS.
Key Messages
The concept of resilience can provide a useful framework for health systems strengthening, if it is reframed to align with the attributes of health systems as complex adaptive systems.
The resilience of health systems is an emergent property that results from the combination of absorptive, adaptive and transformative strategies applied within the system. These strategies are underpinned by cognitive, behavioural and contextual capacities.
Resilience is about (1) everyday resilience, not simply responses to sudden shocks, (2) health system software, not only its hardware and (3) creative adaptation, and transformation, rather than simply bouncing back.
Introduction
The concept of resilience has taken centre stage in global health discourse, catalyzed by major shocks to health systems such as the 2014–2016 Ebola outbreak (Kruk et al. 2015). A central strand of current argument is that resilience reduces the vulnerability of health systems to crisis, by ensuring that they are better prepared for, and effectively respond, to crisis, while at the same time maintaining the delivery of core healthcare services (Kieny et al. 2014; Kruk et al. 2015; Blanchet et al. 2017). However, critics have noted that the application of the concept avoids confronting the political economy forces shaping health systems in low and middle income countries (LMICs), promotes inaction on those forces, and requires that we accept and embrace system vulnerability (Pas 2015; Topp et al. 2016).
We think the different current strands of global health discourse on resilience overlook the transformative potential of nurturing everyday resilience. In this article, we offer our perspective on how the concept of resilience could be re-framed and re-interpreted as everyday resilience, to offer value for health system strengthening. Our perspective, nonetheless, recognizes that efforts to develop ‘a more balanced relation among national states (e.g. balance in trade relations, and structure of aid flows between high income countries and LMICs)’ (Topp et al., 2016) are important to health system strengthening. Indeed, we argue that our understanding of resilience acknowledges power imbalances and might provide the basis for actions to tackle them from within the health system.
Beyond sudden shocks; recognizing everyday resilience
A key characteristic of the current discourse in global health is the framing of resilience as predominantly a response to acute, and often catastrophic shocks to the system (Thomas et al. 2013; Kieny et al. 2014; Kruk et al. 2015). We argue instead, that systems should also be resilient to day-to-day, chronic challenges (Resilient and Responsive Health Systems (RESYST) 2016; Gilson et al. 2017). Frontline managers in LMICs routinely face structural and policy instability, such as changes in governance structures, payment delays, abrupt and imposed policy directives. They also work with unstable authority delegations, manage unpredictable staff, and address changing patient and community expectations. The capacity of health systems to continue to deliver good quality services in the face of these chronic challenges is what we have elsewhere called everyday resilience (Gilson et al. 2017). Everyday resilience emerges from a combination of absorptive, adaptive and transformative strategies, and is underpinned by a set of cognitive, behavioural and contextual capacities (Lengnick-Hall 2005; Resilient and Responsive Health Systems (RESYST) 2016). Cognitive capacity refers to the system’s ability to have an awareness (notice or detect) of a shock or chronic challenge, interpret the challenge (sense making), analyze and understand the challenge and develop appropriate responses to the challenge. Behavioural capacity is about agency. It is the ability of a system to respond to the recognized shock or stress by acting and deploying appropriate strategies. Contextual capacity refers to the resources that can be drawn by the system to exercise both cognitive and behavioural capacities. Everyday resilience has both an inherent, and an instrumental value. In addition to enabling the health system to continuously deliver desirable health outcomes in the face of chronic strain, everyday resilience promotes the system’s ability to respond to sudden shocks.
Resilience is more than bouncing back; appreciating the complex adaptive nature of health systems
The concept of resilience is used in physical, and ecological systems to describe the capacity of a material or system to recover its original state despite external stresses (Folke 2006; MacKinnon and Derickson 2013). This idea of resilience as ‘bouncing back’ has been called resilience engineering, and reflects the quite narrow view that systems are linear and static (Folke 2006). Although not always explicit, this idea seems to underlie the current global health discourse that sees resilience as, essentially, a response to acute and major health system shocks such as disease outbreaks (Kieny et al. 2014; Oxfam 2015). However, health systems are complex adaptive systems (CAS) characterized by, among other attributes, self-organization and emergence (Begun et al. 2003; Agyepong et al. 2012; Kwamie et al. 2014; Prashanth et al. 2014; Barasa et al. 2017). Resilience is an emergent property of CAS, arising from the combination of absorptive, adaptive and transformative strategies applied in managing change by its actors (Béné et al. 2012). The choice of strategy (or mix of strategies) is partly dependent on the nature and scale of the challenge (Béné et al. 2012). A low intensity challenge, such as a short labour strike by a few health workers in an isolated and small region of a country can be dealt with by sanctions and or negotiations (absorptive strategy). Challenges that are of a higher intensity, such as a persistent health workforce unrest across rural areas within a country, exhaust the system’s absorptive capacity and might require an adaptive strategy, such as the introduction of a rural allowance. However, such a strategy might itself generate broader demands for additional payments across the health workforce, through prolonged and recurrent nationwide strikes. This new situation would demand transformative strategies, such as an overhaul of human resource policies, including payment models, schemes of service and recruitment and deployment policies. As this example shows, system adaptations are not always positive. Systems can experience mal-adaptation to undesirable states (Barasa et al. 2017; Gilson et al. 2017). Health systems are resilient when they adapt and transform to support the continued delivery of good quality services and wider action to address emerging health needs appropriately. Within a complexity paradigm, nurturing resilience is about creating the conditions that enable system’s effectiveness—i.e. that enable desirable emergent future states by feeding the natural, bottom-up dynamics of emergence and innovation, rather than by imposing simple and mechanistic, cause and effect type solutions to current problems (Barasa et al. 2017; Gilson et al. 2017).
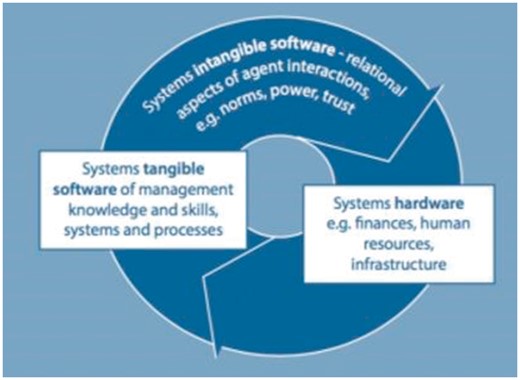
Resilient health systems have well-matched combinations of hardware and software
Complex health systems are comprised of both hardware and software (Sheikh et al. 2011). Hardware includes the familiar ‘building blocks’ such as infrastructure, commodities, human resources and finances (Sheikh et al. 2011). System software includes the tangible software of management knowledge and skills, and organizational systems and procedures as well as the intangible software of values and norms, relationships and power (Figure 1) (Elloker et al. 2012). Global health discourse and action appears biased in favour of hardware—building resilience is sometimes seen as demanding more money, more health workers, more hospitals, better surveillance systems (Oxfam 2015). This hardware bias has perhaps contributed to the criticism that health resilience thinking adopts the view that system actors are naïve, and neutral players, without political interests or influence (MacKinnon and Derickson 2013; Evans and Reid 2015). Applied this way, the concept is unable to capture actors’ power and agency (Béné et al. 2012). However, health system resilience is more about software than hardware. While ensuring that health systems are adequately resourced (with infrastructure, health workers and health commodities) bolsters resilience, effective planning processes, management and leadership capacities (tangible software), and health worker motivation, productive cultures, and healthy power dynamics among system actors (intangible software) are essential for health system resilience (Gilson et al. 2017). A resilience framework that recognizes system software can analyse the influence of both internal and external power dynamics and thus provide the basis for action to strengthen health systems.
Resilience should not incentivize inaction and preserve status quo
Another criticism of resilience as a concept is that is focuses attention on the anticipation of future crises, ensuring that the status quo is maintained (Evans and Reid 2013, 2015; Topp et al. 2016). This criticism is warranted to the extent that resilience is conceptualized in the narrow ‘bouncing back’ engineering sense. However, when the resilience of health systems is conceptualized as an emergent feature of CAS, requiring creative adaptation, learning and transformation, then resilience becomes an active process within a dynamic health system that is constantly navigating challenges by becoming better. Far from favouring the status quo and incentivizing inaction, a resilient health system actively steers towards the state that continues to deliver good quality healthcare services within a changing environment. From the CAS perspective, resilience thinking, far from promoting inaction, promotes agency and the search for adaptive and transformative approaches to respond to health system strain. Indeed, such strategies would include the wider action needed to address the wider political economy influences that shape both the goals and dynamics of health systems.
Resilience does not mean submitting to a dystopian reality
Resilience discourse inside and outside the health sector has also been criticized as requiring that we accept as the new normal a view of the world as permanently in crisis and exposed to endemic dangers (Evans and Reid 2013, 2015; Pas 2015). Resilience is seen as replacing the quest for a safe and secure future, with acceptance of powerlessness and the reality of life in a dystopian world (Reid 2010; Evans and Reid 2013; Pas 2015). In the health sector, such an interpretation of the concept would require health system actors to abandon the dream of ever achieving secure and responsive health systems and instead, to embrace vulnerability. This criticism is unwarranted and again based on the conception of resilience in static, linear systems. It represents a denial of the reality of health systems as CAS and hence characterized by uncertainty. Appreciating uncertainty is not synonymous with acquiescing to helplessness and vulnerability. On the contrary, from the CAS perspective, resilience thinking adopts a pragmatic view of the challenges that health systems face. It embraces the uncertainty of challenges, changing context and complexity of interventions. Because CAS are characterized by uncertainty and surprise, health system actors must learn to manage by change rather than simply reacting to it, or denying it (Walker et al. 2004; Folke 2006). Rather than seeking to control change in systems assumed to be stable, they must manage the capacity of health systems to cope with, adapt to, and shape change (Adger 2003; Berkes et al. 2003; Folke 2006).
Conclusion
As Kruk et al. (2015) observe, resilient health systems could yield a ‘resilience dividend’, where good health outcomes are produced both in periods of crisis and in periods without crisis. However, for this to be realized there is a need to reframe the application of the concept to fit with the attributes of health systems as CAS. We argue that health system actors should (1) embrace the notion of resilience as going beyond responses to sudden shocks, and encompassing everyday resilience, (2) view health systems as comprised of both system software and hardware and (3) conceptualize health system resilience as being about creative adaptation and transformation, not simply bouncing back.
Conflict of interest statement. None declared.
Acknowledgements
We thank our colleagues in Kenya and South Africa who have worked with us in developing the ideas underlying this commentary. This study is published with the permission of the Director of KEMRI.
Funding
Edwine Barasa is supported by a Wellcome Trust Training Fellowship (#107527). Edwine W. Barasa, and Lucy Gilson are members of the Consortium for Resilient and Responsive Health Systems (RESYST). This document is an output from a project funded by the UK Aid from the UK Department for International Development (DFID) for the benefit of developing countries. However, the views expressed and information contained in it are not necessarily those of or endorsed by DFID, which can accept no responsibility for such views or information or for any reliance placed on them. The funders had no role in the writing of this paper or in the decision to submit for publication.