Abstract
Neonatal units in teaching and non-teaching hospitals both in public and private hospitals have been increasing in number in the country since the sixties. In 1994, a District Newborn Care Programme was introduced as a part of the Child Survival and Safe Motherhood Programme (CSSM) in 26 districts. Inpatient care of small and sick newborns in the public health system got a boost under National Rural Health Mission with the launch of the national programme on facility-based newborn care (FBNC). This has led to a nationwide creation of Newborn Care Corners (NBCC) at every point of child birth, newborn stabilization units (NBSUs) at First Referral Units (FRUs) and special newborn care units (SNCUs) at district hospitals. Guidelines and toolkits for standardized infrastructure, human resources and services at each level have been developed and a system of reporting data on FBNC created. Till March 2015, there were 565 SNCUs, 1904 NBSUs and 14 163 NBCCs operating in the country. There has been considerable progress in operationalizing SNCUs at the district hospitals; however establishing a network of SNCUs, NBSUs and NBCCs as a composite functional unit of newborn care continuum at the district level has lagged behind. NBSUs, the first point of referral for the sick newborn, have not received the desired attention and have remained a weak link in most districts. Other challenges include shortage of physicians, and hospital beds and absence of mechanisms for timely repair of equipment. With admission protocols not being adequately followed and a weak NBSU system, SNCUs are faced with the problem of admission overload and poor quality of care. Applying best practices of care at SNCUs, creating more NBSU linkages and strengthening NBCCs are important steps toward improving quality of FBNC. This can be further improved with regular monitoring and mentoring from experienced pediatricians, and nurses drawn from medical colleges and the private sector. In addition there is a need to further increase such units to address the unmet need of facility-based care.
Similar content being viewed by others
Background
Facility-based newborn care (FBNC) refers to round-the-clock clinical services provided by skilled personnel at healthcare facilities.1, 2 Historically, the care of small and sick newborn babies has always been at the secondary or tertiary care units situated in the hospitals (for example, neonatal intensive care units). In India, facility care for newborns began in the early 1960s in a few teaching hospitals; however, the expansion of these services was tardy until the 1980s.3 Thereafter the pace picked up in both the private sector and the larger public sector hospitals, and the first secondary care newborn unit in the public health system was established in late 1980’s in a district in Tamil Nadu.3
During the decade of 1990 to 2000, the country recognized the importance of newborn health at the public healthcare facilities. For the first time under a national programme, a package of interventions for Essential Newborn Care (breast feeding, warmth and hygiene) organized at different levels of the health system was introduced.4 This package was expanded and strengthened in subsequent national programs by adding other components of newborn health.5 The country’s leading professional association National Neonatology Forum (NNF) in neonatal health established accreditation norms for quality newborn care at health facility. In 1994 FBNC became functional in 26 districts with strengthening of district and sub-district health facilities mainly through provision of equipment (radiant warmers, resuscitation equipment, weighing scale and phototherapy units), trainings and oversight.6
The feasibility of establishing and operating a district-level unit for the care of small and sick newborns was first demonstrated in 2003 in Purulia district of West Bengal.7 The unit, known as special newborn care unit (SNCU), was established at the district hospital by a non-profit organization, technically and financially supported by UNICEF and managed with the help of relocated staff from within the district. NMR among the admitted newborns reduced by 14% in the first year and by 21% in the second year after the SNCU became functional. At the population level, this was estimated to have led to a reduction of NMR by ~10% in the district in 2 years.8 With this, the present concept of FBNC was born.
With the launch of the National Rural Health Mission (NRHM) in 2005, the focus on newborn care became central to the child health strategy of the government. Subsequent increase in institutional deliveries after the introduction of conditional cash transfer scheme made it even more necessary to invest in facility care of the newborn. The Government of India adapted the Purulia district model for as a national model by operationalizing SNCUs at district levels and extending the care of sick newborns to the sub-district levels through the establishment of Newborn Stabilization Units (NBSUs) at the First Referral Units and Community Health Centres. In addition, a dedicated space (known as Newborn Care Corner or NBCC) was ensured at all delivery points for strengthening essential newborn care and resuscitation. UNICEF India played a key role in partnership with the state governments in the early operationalization and expansion of this program in the country.
Structure of delivery of FBNC
Newborn care facilities at different levels
The facility based care for newborns has two components, that is, essential newborn care for all and care of sick newborns. For providing these services, three levels of newborn care have been defined in literature.2, 9, 10, 11 The complexity of management of sick newborns has been used to define the level of care that can be provided at different healthcare facilities. The services provided at each level is a product of infrastructure, availability of skilled manpower and referral capacity of the institution.12
The services to be provided and infrastructural requirements at different levels under NRHM are summarized in Table 1.12 Operational guidelines for FBNC have been developed to provide detailed information about the design, infrastructure, equipment, manpower, data collection system and newborn care protocols.12, 13 These guidelines are made accessible to those involved in managing and implementing the program.
Emergency obstetric care services
Facility-based care of neonates is closely associated with obstetric services. Skilled birth attendance must be ensured at all points of child birth, and emergency obstetric care (EmOC) ensured where neonates receive secondary and tertiary care. Access to EmOC has a critical role to play in reducing neonatal mortality.14, 15 EmOC includes services aimed at improving the availability, accessibility, quality and use of services for the treatment of complications that arise during pregnancy. There are two levels of EmOC, namely, the basic EmOC, and the comprehensive EmOC. It is recommended that a population of 500 000 should have five EmOC-providing facilities, with at least one providing comprehensive EmOC.16
Janani suraksha yojana (JSY)
The need for FBNC has increased further since the introduction of JSY, a cash transfer incentive scheme for promoting institutional deliveries, in 2005.17 The goals are to reduce the overall maternal and infant mortality rates and to ensure 100% institutional deliveries in the underprivileged sections of the population (those living below poverty line, scheduled caste and tribes).18
The program focuses on poor pregnant woman with special dispensation for states having low institutional delivery rates and high burden of maternal and neonatal mortality, namely Uttar Pradesh, Uttarakhand, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Assam, Rajasthan, Odisha, and Jammu and Kashmir. The benefits are linked to availing of antenatal check-ups by the pregnant woman and getting her delivery conducted in a healthcare facility. Although the beneficiaries are encouraged to register themselves with the health workers at the subcentres, Anganwadis or PHCs for availing of at least four antenatal check-ups, postnatal care and neonatal care, the disbursement of enhanced benefits are linked to institutional delivery18 (Table 2).
JSY, however, does not address the issues regarding a woman’s socio-economic compulsion to work right up to the last stage of pregnancy and resuming work soon after child birth. Hence, a need for introducing a modest maternity benefit to partly compensate for their loss of wages was recommended by the Planning Commission in the XIth Five Year Plan.19
In view of the above, the Ministry of Women and Child Development (MWCD) formulated a new program for pregnant and lactating mothers called Indira Gandhi Matritva Sahyog Yojana (IGMSY) – a Conditional Maternity Benefit Scheme. The scheme launched in 2010 on a pilot basis in 52 selected districts of the country provides a cash incentive of INR 4000 directly to women aged above 19 years for the first two live births subject to the woman fulfilling specific conditions relating to maternal child health and nutrition. Cash incentive is provided in three installments between the second trimester of pregnancy and till the infant completes 6 months of age. Women enrolled under IGMSY are encouraged to avail of the JSY package also for institutional delivery and vice-versa. However, there is no cash incentive under IGMSY at the time of delivery since cash incentive for this is already provided under JSY.19
Implementation status of FBNC and outcome
The country has witnessed a huge increase in terms of FBNC in the past 10 years. Since the time the first model was set up in 2003, the number of facilities has grown exponentially. Guidelines and protocols have been developed in accordance with the IPHS standards to guide the entire process of expansion. A strong political commitment has enabled the states to take forward the agenda of FBNC.
Till March 2015, 565 SNCUs, 1904 NBSUs and 14 163 NBCCs were functional in the country (Table 3). States like Madhya Pradesh, Rajasthan and Andhra Pradesh have established SNCUs in all their districts although the distribution of functional NBSUs at the First Referral Units/Community Health Centres level is a concern. A total of 8473 beds were available in SNCUs. More than 600 000 babies were admitted during the year 2014–15.20, 21, 22, 23, 24
Several assessments have been undertaken by various agencies and organizations to assess the functionality and utilization of SNCUs.20, 25, 26, 27, 28, 29, 30, 31, 32, 33 Clearly, the utilization of services in these units has increased over time. Most of the SNCUs (86%) in weaker states have bed strength of 12 or more, while the proportion of such units in relatively developed states is over 73%.20 Out-born babies constituted 38% of the total admissions according to latest reports. Low birth weight babies made up more than half of total admissions (55%) and these included 14% very low birth weight babies. The main reasons for admission to SNCU were birth asphyxia (22%), sepsis (18%), respiratory distress due to prematurity (15%) and other complications (18%) like hypothermia, congenital malformations and other causes of respiratory distress.
Surveys of facility readiness to deliver essential care were also evaluated. On the whole, the infrastructure, essential drugs and supplies were average, and knowledge of care providers was less than satisfactory. However, skills were predominantly poor and infection control measures required urgent attention.26, 31, 32, 33, 34
Although the overall mortality in SNCUs is ~11%, there is a need to assess the impact of this intervention on reducing neonatal mortality at the population level. 24
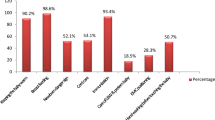
One of the most significant impacts of JSY is the sudden and sharp increase in institutional deliveries, as evident from various nationwide and state/district surveys and analyses (Figure 1). The proportion of institutional deliveries was only half (34.5%, sample registration system, 2005) when the JSY was launched as compared with more recent data (74.4%, sample registration system, 2013).35, 36
Increase in Institutional deliveries following launch of JSY scheme. Source: adapted with permission from Registrar General of India.35, 36 Sample registration system (SRS) statistical report 2005 and 2013. Available from: http://www.censusindia.gov.in/vital_statistics/SRS_Reports_2013.html, Copyright 2013, Office of the Registrar General and Census Commissioner, India.
Implementation challenges of facility-based care and opportunities
There has been a huge investment and expansion of facility based newborn care in the country. Several assessments have been undertaken to analyze the strengths and barriers within the system. Most studies indicate that infrastructure has been well developed over the past decade and simultaneously delivery of services has also increased. However, quality of services is a concern. This is due to a range of challenges that the system is facing.
Lack of adequate and skilled manpower
Adequacy of human resources was a concern with only 53% units having an adequate number of physicians and <50% having an adequate number of nurses.20Apart from the low numbers of trained people, retention of the existing pool of trained people is an emerging problem. This is mainly attributed to low pay, lack of incentives to work in rural areas, absenteeism (because of private practice) and brain drain.37
Almost half of all the SNCUs have inadequate nurses and physicians.25, 29 Availability of physicians is not an issue but many of them are multi-tasking and involved in other activities besides their role in SNCUs. In the absence of an adequate pool of physicians, they are mobilized from the PHCs leaving those positions vacant. It is also known that despite advertisements for physicians to be appointed on a contractual basis, they refuse to join because of the absence of clearcut guidelines about promotions and financial benefits.38 Madhya Pradesh is an example of a state which has used a mix of contractual and regular physicians and nurses to tackle the issue of HR shortage.
The quality of care in a facility is the outcome of trained personnel, adherence to guidelines and adequate manpower. Good quality training of personnel involved in delivery of newborn care is the key solution and guidelines are in place, but these have not kept pace with the demand of expansion. Although some studies indicate that the duration of training is different from what is advocated by NNF, there are others that have shown that staff has been put on a job without any formal training.25, 31, 32
A possible solution is task shifting. Medical officers can be trained to manage an SNCU effectively. Fellows who are trained for 1 year in recognized centers by NNF is also an effective strategy. Sites where availability of nursing staff is a problem, nursing aides can be utilized. Ongoing mentoring is absolutely necessary to keep the knowledge and motivation level high.
Issue of functional equipment
The neonatal services are equipment-driven services. The reasons behind poor functionality of equipment are the following: poor quality supplies, lack of power backup for the SNCUs (not relying on the hospital generator), absence of annual maintenance contract (both preventive and maintenance), delay in repair of equipment, absence of local biomedical engineers and lack of training on how to use equipment.39 In many states availability of equipment is also an issue with many of the SNCU’s equipment not being included in the government rate contract. This has delayed scale up of the program in the states of Jharkhand, Chhattisgarh and North East states.
Engaging biomedical engineers at the district level and local engineers for repair of equipment and trouble-shooting are some key solutions. Training of cold chain handlers who are available in every district on maintenance of SNCU equipment’s can be one of the options; this has been piloted by UNICEF in collaboration with National cold chain training centre, Pune. It is important to earmark some funds for this activity that can be utilized by the officer in-charge without going through administrative hassles. Regular audits and accreditation of facilities can also address these problems.
Admission overload
Various assessments have reported admission overload leading to difficulty in delivering quality newborn care services. The prime reasons behind this – apart from the vast number of admissions – are lack of adherence to admission and discharge guidelines and inability to refuse admissions on social or moral grounds. Institutional deliveries have increased and so has the demand for FBNC. This has resulted in sharing of beds by already vulnerable neonates. Clearly, if the pressure to admit more babies is there, there is a possibility of these babies being discharged prematurely which often leads to a higher re-admission rate and increased risk of death.
The average length of stay is another component that influences the quality of care. This is further aggravated as the FBNC is not developed as a three-tier system.
It is estimated that for a one million population of a district (with a crude birth rate of 20/1000 population, 8–10% babies requiring special care with 2 to 3% of them in intensive care and the average length of stay of 5 days), the total number of beds required in a district would be 55–60.10, 11 Assuming that the private sector may provide some proportion of these beds, the number of existing beds in the public sector SNCUs is still short of the estimates. Ultimately, each district would require additional SNCUs to cater to sick newborns.24, 25, 29
It is important to assess the reasons for non-adherence to admission and discharge protocols by the physicians and nurses and take corrective actions. A Kangaroo Mother Care (KMC) unit of six to ten beds in every facility can provide quality care to stable small babies and reduce the admission overload. Involving mothers in care giving not only has immense potential to improve quality of care, but also helps in reducing the work load of nurses.
Poor adherence to infection control
Infection control protocols have been developed but adherence to them is a challenge.25, 27, 29, 31 This could be due to different reasons related either to the attitude of the health staff but more commonly to the lack of adequate number of cleaning staff, admission overload, less number of hand-washing facilities inside the unit and so on.
Ability of the healthcare staff to adhere to infection control practices is also affected by the quality of their training 25 Ensuring the availability of running water and use of alcohol hand rub are some of the simple solutions. On the site surprise checks and CCTV monitoring would also be useful.
Inadequate post-discharge care and follow up
A follow up study of more than 2000 newborns discharged from SNCUs was conducted by UNICEF and Government of MP in 2010 to evaluate the long-term survival of these babies. The results showed 10.2% mortality at 1 year of age in those babies who were successfully discharged after completion of their treatment.40 It was therefore suggested to link SNCU care to a strong follow up and home care program.12 In some states such as Madhya Pradesh, follow-up of SNCU discharged babies is ensured through a mobile phone enabled tracking system in which mothers and ASHAs are connected to the unit for follow-up contacts. There is a need to now replicate this model in other parts of the country.
Inequitable access to both girls and boys
Gender bias results in discrimination against and fewer admissions for sick females leading to disproportionately more male babies being admitted in health facilities. Data from select states have shown that male admissions outnumbered the female admissions.20 Another study has shown that more female infants die compared with males following post-delivery discharge from a healthcare facility.41
The problem of differential care seeking has to be addressed by a comprehensive approach targeting the community, healthcare facility and at the individual level. To ensure equitable access, it is vital to track and monitor reports/data disaggregated by gender. Health professionals working at facilities should be sensitized toward this practice and make sure that female neonates do not face any barrier to care.
Affordability barriers for the poor
Key barriers to accessing affordable treatment include low income/resources of family, corrupt practices of staff and the high cost of private sector care. Despite an increase in the number of institutional deliveries, many pregnant women either hesitate to access health facilities or, if they do, they are not willing to stay for 48 h after delivery. 42 Usually services at the public healthcare facilities are available at no or minimal cost. Yet there are studies indicating that families spend money on treatment of babies even if they are admitted to public facilities. Exit interviews conducted in Punjab and Odisha showed that most antibiotics for sick newborns were purchased from outside.27
In June 2011, the Union Ministry of Health and Family Welfare launched the Janani Shishu Suraksha Karyakram (JSSK) program that emphasizes on entitlements and aims to eliminate out-of-pocket medical expenditure for both pregnant women and sick neonates.42 The scheme envisages free and cashless services to pregnant women and includes normal deliveries, cesarean operations, and also treatment of sick newborns and infants (up to 1 year after birth) in all government health institutions across all states/UTs. Although there are provisions for free treatment of poor/marginalized families, but unfortunately these families seek or receive adequate information about this at the time of admission.
Monitoring FBNCs
Efficient mechanisms to capture monitoring data, analyze and utilize it for programmatic improvement is essential to improve the status of FBNC. Maintenance of records as well as transmission of information at various levels in the system is a critical challenge. Unavailability of uniform guidelines and lack of awareness and motivation were the major hurdles in the way of efficient data management initially. However, with the current thrust that is being laid on this component, uniform guidelines have been disseminated to the states and as a result the reporting system has improved.43 Besides, medical colleges have been identified as National and Regional Collaborating Centers for capacity building, mentoring and supervision of SNCUs.12
Data reporting from SNCU are often delayed with a long-lag period between reports being received and feedback shared with districts and state. To address this, UNICEF supported National Health Mission (NHM) to develop a real-time online monitoring system which was first piloted in Madhya Pradesh and is being scaled up across the country under the India Newborn Action Plan (INAP). The system monitors performance of SNCUs and tracks follow-up till 1 year of age. Currently 11 states and more than 300 SNCUs are reporting online.24
In addition, supervisory and monitoring checklists are available for assessing the key parameters in a standard manner with ease. Checklist-based interventions aid management of complex or neglected tasks and have been shown to improve performance of health systems. Results from a pilot study conducted in 2010 over a 6-month period at a district level birth subcentre in Karnataka, has shown that these checklists can help in markedly improving delivery of healthcare practices.44
Conclusion
The number of SNCUs, NBSUs and NBCCs has grown at a very rapid pace; however, the quality of care is variable. Guidelines and protocols on FBNC are currently in place and are often adhered to. The linkages of SNCUs with NBSUs and NBCCs are weak thus hampering the continuum of newborn care. NBSUs have not received the required attention and have remained a weak link in most districts. Increased demand for services coupled with absence of an intermediate level has resulted in an overload at SNCUs. Shortage of doctors and beds, and absence of mechanisms for timely repair of equipment are common challenges.
Recommendations
-
Take measures to diffuse best practices from states/districts with well-functioning FBNC to states/districts with poor coverage and quality; create opportunities for this cross learning.
-
Establish sustainable quality assurance systems for FBNC in all states to ensure high standards of care.
-
Engage medical colleges’ faculty and other eminent pediatricians to mentor quality FBNC.
-
Build effective scale up of KMC on the existing platform of FBNC.
-
Ensure staff policies that support retention and motivation of the staff; address negative aspects of contractual appointments, low remuneration, lack of career progression and other issues.
-
Strengthen the model of NBSU (by integrating KMC facilities, standardizing protocols and having a follow-up system in place) to make this level of FBNC more functional and effective.
-
Strengthen linkages between SNCUs, NBSUs and PHCs.
-
Improve skills and motivation of care providers to follow standard algorithms and protocols.
-
Ensure quality home care and follow-up of babies after discharge from facilities.
-
Conduct situational analysis of neonatal care services in the private sector and assess scope to improve their quality.
-
Consider engaging private facilities in providing neonatal care through public–private partnership.
-
Consider involving more medical colleges for mentoring and improving the quality of facility based newborn care.
-
Invest in operations research to improve quality of care and neonatal outcomes at the facilities.
References
Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 2005; 365: 977–988.
Neogi SB, Malhotra S, Zodpey S, Mohan P . Does facility-based newborn care improve neonatal outcomes? A review of evidence. Indian Pediatr 2012; 49: 651–658.
Singh M, Paul V, Deorari A . The state of India's neonatal units in the mid-nineties. Indian Pediatr 1997; 34: 696–701.
Child Health Programme, Ministry of Health and Family Welfare, Government of India. Child survival and safe motherhood (CSSM) programme. Available from: mohfw.nic.in/WriteReadData/l892s/6342515027file14.pdf (accessed on 6 April 2016).
Ramji S, Modi M, Gupta N . 50 years of neonatology in India: progress and future. Indian Pediatr 2013; 50: 104–106.
Jhpiego Shaping policy for maternal and newborn health: a compendium of case studies, 2003. Available from http://www.jhpiego.org/files/MNHPolComp.pdf (accessed on 31 October 2013).
Sen A, Mahalanabis D, Singh AK, Som TK, Bandyopadhyay S . Development and effects of a neonatal care unit in rural India. Lancet 2005; 366: 27–28.
Sen A, Mahalanabis D, Singh AK, Som TK, Bandyopadhyay S . Impact of a district level sick newborn care unit on neonatal mortality rate: 2-year follow-up. J Perinatol 2008; 29: 150–155.
Gould JB, Marks AR, Chavez G . Expansion of community-based perinatal care in California. J Perinatol 2002; 22: 630.
Bhakoo ON, Kumar P . Current challenges and future prospects of neonatal care in India. Indian J Pediatr 2013; 80: 39–49.
PHFI, UNICEF, NNF. Organization of newborn care. Facility based newborn care - current situation and future directions. Round table consultation, 2010.
Ministry of Health and Family Welfare, Government of India. Facility based newborn care: operational guidelines, 2011.
UNICEF. Toolkit for setting up special care newborn units, stabilisation units and newborn care corners. Available from http://www.unicef.org/india/SCNU_book1_April_6.pdf (accessed on 31 October 2012).
Rammohan A, Iqbal K, Awofeso N . Reducing neonatal mortality in India: critical role of access to emergency obstetric care. PLos One 2013; 8: e57244.
Indian public health standards. Available from http://nrhm.gov.in/about-nrhm/guidelines/indian-public-health-standards.html (accessed on 14 Feb 2013).
Monitoring emergency obstetric care. Available from www.unfpa.org/publications/monitoring-emergency-obstetric-care (accessed on 14 Feb 2013).
MoHFW National Rural Health Mission Directory of Innovations Implemented in the Health Sector. MoHFW, Government of India: New Delhi, 2009.
MoHFW Janani Suraksha Yojna Guidelines for Implementation. Government of India: New Delhi, 2006. Available from www.mohfw.nic.in.
Indira Gandhi Matritva Sahyog Yojna - A Conditional Maternity Benefit Scheme, Ministry of Women and Child Development, Government of India. April 2011. Available from: http://wcd.nic.in/sites/default/files/IGMSYscheme.pdf. (Accessed on 30 September 2016).
Child Health Division, Ministry of Health and Family Welfare, Government of India. Two year progress report of special newborn care units in India, 2013.
Ministry of Health and Family Welfare, Government of India. Rural health statistics, 2011.
Child Health and Immunization Division, Ministry of Health and Family Welfare, Government of India. Monthly programme monitoring sheets, 2013. Available from http://www.nrhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/guidelines.html.
Ministry of Health and Family Welfare, Government of India. Annual Report of Department of Health and Family Welfare for the year 2013-14. Available from www.mohfw.nic.in (accessed on 20 January 2015).
State-wise progress under NRHM (as on March 2015)Child Health Division, Ministry of Health and Family Welfare. Government of India. Available from http://nrhm.gov.in/nrhm-components/rmnch-a/child-health-immunization.html?id=405.
Public Health Foundation of India. An evaluation of special care newborn units in eight districts of India - a report, 2010.
Neogi SB, Malhotra S, Zodpey S, Mohan P . Challenges in scaling up of special care newborn units-lessons from India. Indian Pediatr 2011; 48: 931–935.
Delloite. Supported by MoHFW and Department for International Development. Evaluation of skill based child health trainings - a report, 2013.
National Rural Health Mission, Ministry of Health and Family Welfare, Government of India. Sixth Common Review Mission, 2012.
Government of Andhra Pradesh. National Rural Health Mission, UNICEF. Report of assessment of FBNC in Andhra Pradesh with special focus on special newborn care units. National Rural Health Mission, Government of Andhra Pradesh and UNICEF 2012.
National Health Systems Resource Centre. Government of India. As-is report, special newborn care unit, 2012.
Ministry of Health and Family Welfare. Government of India. Rapid assesment of NBSUs and NBCCs in India, 2013.
Indian Institute of Public Health. Effect of Facility Based Neonatal Care Interventions in Nagaur and Chattarpur Districts - A Report. Public Health Foundation of India: New Delhi,, 2012.
Facility readiness assessment; Haryana, UP, Jharkhand. MCHIP report. 2012–13.
PHFI, UNICEF and State Health Society. Management of facility based newborn care in Bihar, 2012.
Registrar General of India. Sample registration system (SRS) statistical report 2005. New Delhi, 2013.
Registrar General of India. Sample registration system (SRS) statistical report 2013. New Delhi, 2013.
New Delhi: a joint publication of Indian Institute of Public Health Delhi, Public Health Foundation of India, UNICEF, National Neonatology Forum. Human resources for facility-based newborn care in India. Issues and options, 2010.
Neogi SB, Malhotra S, Zodpey S, Mohan P . Assessment of special care newborn units in India. J Health Popul Nutr 2011; 29: 500.
New Delhi: a joint publication of Indian Institute of Public Health-Delhi, Public Health Foundation of India, UNICEF and National Neonatology Forum. Optimal utilization of equipment at special care newborn units - issues and solutions, 2010.
UNICEF. Innovative approaches to maternal and newborn health. Compendium of case studies. Available at www.unicef.org/health/files/Innovative_Appproaches_MNH_CaseStudies-2013.pdf (accessed on 16 June 2015).
Malhotra S, Neogi SB, Raj SS, Sharma K, Zodpey SP . Tracking survival of institutional births for neonatal period-feasibility at district hospitals. Indian Pediatr 2012;. 49: 479–480.
National Rural Health Mission, Ministry of Health and Family Welfare.Government of India. Guidelines for JananiShishuSurakshaKaryakram, 2011.
Ministry of Health and Family Welfare. Government of India. National rural health mission, state wise progress, 2013.
Spector JM, Agrawal P, Kodkany B, Lipsitz S, Lashoher A, Dziekan G et al. Improving quality of care for maternal and newborn health: prospective pilot study of the WHO safe childbirth checklist programme. PLoS One 2012; 7: e35151.
Acknowledgements
Support for this publication was provided by Save the Children’s Saving Newborn Lives program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Rajesh Khanna is affiliated to Saving Newborn Lives, Save the Children, India (sponsor of the supplement). The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Neogi, S., Khanna, R., Chauhan, M. et al. Inpatient care of small and sick newborns in healthcare facilities. J Perinatol 36 (Suppl 3), S18–S23 (2016). https://doi.org/10.1038/jp.2016.186
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.186
This article is cited by
-
Turning the Gaze from Survive to Thrive for Children in India: Learnings from Two Case Studies
Indian Journal of Pediatrics (2023)
-
Care of Healthy as well as Sick Newborns in India: A Narrative Review
Indian Journal of Pediatrics (2023)
-
Feasibility, Sustainability, and Effectiveness of the Implementation of “Facility-Team-Driven” Approach for Improving the Quality of Newborn Care in South India
Indian Journal of Pediatrics (2023)
-
Quality of care assessment for small and sick newborns and young infants in Pakistan: findings from a cross-sectional study
BMC Pediatrics (2022)
-
An analysis of the impact of newborn survival policies in Pakistan using a policy triangle framework
Health Research Policy and Systems (2021)