Abstract
Objective:
Sick young infants are at high risk of mortality in developing countries, but families often decline hospital referral. Our objective was to identify the predictors of acceptance of referral for hospital care among families of severely ill newborns and infants <59 days old in three low-income communities of Karachi, Pakistan.
Study Design:
A cohort of 541 newborns and infants referred from home by community health workers conducting household surveillance, and diagnosed with a serious illness at local community clinics between 1 January and 31 December 2007, was followed-up within 1 month of referral to the public hospital.
Result:
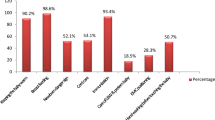
Only 24% of families accepted hospital referral. Major reasons for refusal were financial difficulties (67%) and father/elder denying permission (65%). Religious/cultural beliefs were cited by 20% of families. Referral acceptance was higher with recognition of severity of the illness by mother (odds ratio=12.7; 95% confidence interval=4.6 to 35.2), family's ability to speak the dominant language at hospital (odds ratio=2.0; 95% confidence interval=1.3-3.1), presence of grunting in the infant (odds ratio=3.3; 95% confidence interval=1.2-9.0) and infant temperature <35.5 °C (odds ratio=4.1; 95% confidence interval=2.3 to 7.4). No gender differential was observed.
Conclusion:
Refusal of hospital referral for sick young infants is very common. Interventions that encourage appropriate care seeking, as well as community-based management of young infant illnesses when referral is not feasible are needed to improve neonatal survival in low-income countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Lawn JE, Cousens S, Zupan J . 4 million neonatal deaths: when? where? why? Lancet 2005; 365 (9462): 891–900.
Bryce J, Daelmans B, Dwivedi A, Fauveau V, Lawn JE, Mason E et al. Countdown to 2015 for maternal, newborn, and child survival: the 2008 report on tracking coverage of interventions. Lancet 2008; 371 (9620): 1247–1258.
Hyder AA, Wali SA, McGuckin J . The burden of disease from neonatal mortality: a review of South Asia and Sub-Saharan Africa. Bjog 2003; 110 (10): 894–901.
NIPS. Pakistan Demographic and Health Survey 2006-07. In. National Institute of Population Studies and Macro International Inc: Islamabad, Pakistan:, 2008.
Terra de Souza AC, Peterson KE, Andrade FM, Gardner J, Ascherio A . Circumstances of post-neonatal deaths in Ceara, Northeast Brazil: mother's health care-seeking behaviors during their infant's fatal illness. Soc Sci Med 2000; 51 (11): 1675–1693.
Bang AT, Bang RA, Baitule S, Deshmukh M, Reddy MH . Burden of morbidities and the unmet need for health care in rural neonates—a prospective observational study in Gadchiroli, India. Indian Pediatr 2001; 38 (9): 952–965.
Amarasiri de Silva MW, Wijekoon A, Hornik R, Martines J . Care seeking in Sri Lanka: one possible explanation for low childhood mortality. Soc Sci Med 2001; 53 (10): 1363–1372.
D’Souza RM . Role of health-seeking behaviour in child mortality in the slums of Karachi, Pakistan. J Biosoc Sci 2003; 35 (1): 131–144.
Reyes H, Perez-Cuevas R, Salmeron J, Tome P, Guiscafre H, Gutierrez G . Infant mortality due to acute respiratory infections: the influence of primary care processes. Health Policy Plan 1997; 12 (3): 214–223.
Sutrisna B, Reingold A, Kresno S, Harrison G, Utomo B . Care-seeking for fatal illnesses in young children in Indramayu, west Java, Indonesia. Lancet 1993; 342 (8874): 787–789.
Balabanova D, McKee M, Pomerleau J, Rose R, Haerpfer C . Health service utilization in the former soviet union: evidence from eight countries. Health Serv Res 2004; 39 (6 Part 2): 1927–1950.
Baqui AH, Black RE, Arifeen SE, Hill K, Mitra SN, al Sabir A . Causes of childhood deaths in Bangladesh: results of a nationwide verbal autopsy study. Bull World Health Organ 1998; 76 (2): 161–171.
D’Souza R M, Bryant JH . Determinants of childhood mortality in slums of Karachi, Pakistan. J Health Popul Dev Ctries 1999; 2 (1): 33–44.
Janjua NZ, Khan MI, Usman HR, Azam I, Khalil M, Ahmad K . Pattern of health care utilization and determinants of care-seeking from GPs in two districts of Pakistan. Southeast Asian J Trop Med Public Health 2006; 37 (6): 1242–1253.
Scarpaci JL . Help-seeking behavior, use, and satisfaction among frequent primary care users in Santiago de Chile. J Health Soc Behav 1988; 29 (3): 199–213.
Taffa N, Chepngeno G, Amuyunzu-Nyamongo M . Child morbidity and healthcare utilization in the slums of Nairobi, Kenya. J Trop Pediatr 2005; 51 (5): 279–284.
Teerawichitchainan B, Phillips JF . Ethnic differentials in parental health seeking for childhood illness in Vietnam. Soc Sci Med 2008; 66 (5): 1118–1130.
Van der Stuyft P, Sorensen SC, Delgado E, Bocaletti E . Health seeking behaviour for child illness in rural Guatemala. Trop Med Int Health 1996; 1 (2): 161–170.
Green M . Public reform and the privatisation of poverty: some institutional determinants of health seeking behaviour in southern Tanzania. Cult Med Psychiatry 2000; 24 (4): 403–430.
de Zoysa I, Bhandari N, Akhtari N, Bhan MK . Careseeking for illness in young infants in an urban slum in India. Soc Sci Med 1998; 47 (12): 2101–2111.
Kamat VR . ‘I thought it was only ordinary fever!’ cultural knowledge and the micropolitics of therapy seeking for childhood febrile illness in Tanzania. Soc Sci Med 2006; 62 (12): 2945–2959.
Taffa N, Chepngeno G . Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health 2005; 10 (3): 240–245.
YICSSG. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet 2008; 371 (9607): 135–142.
Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet 2008; 371 (9628): 1936–1944.
Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM et al. Effect of a participatory intervention with women′s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet 2004; 364 (9438): 970–979.
Willis JR, Kumar V, Mohanty S et al. Gender differences in perception and care-seeking for illness of newborns in rural Uttar Pradesh, India. J Health Popul Nutr 2009; 27 (1): 62–71.
McMillen MM . Differential mortality by sex in fetal and neonatal deaths. Science 1979; 204 (4388): 89–91.
Ulizzi L, Zonta LA . Sex differential patterns in perinatal deaths in Italy. Hum Biol 2002; 74 (6): 879–888.
Danso-Appiah A, De Vlas SJ, Bosompem KM, Habbema JD . Determinants of health-seeking behaviour for schistosomiasis-related symptoms in the context of integrating schistosomiasis control within the regular health services in Ghana. Trop Med Int Health 2004; 9 (7): 784–794.
Mohan P, Iyengar SD, Agarwal K, Martines JC, Sen K . Care-seeking practices in rural Rajasthan: barriers and facilitating factors. J Perinatol 2008; 28 (Suppl 2): S31–S37.
Goodburn EA, Gazi R, Chowdhury M . Beliefs and practices regarding delivery and postpartum maternal morbidity in rural Bangladesh. Stud Fam Plann 1995; 26 (1): 22–32.
Dongre AR, Deshmukh PR, Garg BS . Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha. Indian J Pediatr 2008; 75 (4): 325–329.
Syed U, Khadka N, Khan A, Wall S . Care-seeking practices in South Asia: using formative research to design program interventions to save newborn lives. J Perinatol 2008; 28 (Suppl 2): S9–13.
Edmond K, Zaidi A . New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med; 2010; 7 (3): e1000213.
Acknowledgements
A Owais and S Sultana are supported by a grant from the Fogarty International Center, National Institute of Health, USA (Grant number: ID43 TW0075 85-01). This study also received funding support from the World Health Organization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Owais, A., Sultana, S., Stein, A. et al. Why do families of sick newborns accept hospital care? a community-based cohort study in Karachi, Pakistan. J Perinatol 31, 586–592 (2011). https://doi.org/10.1038/jp.2010.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.191
Keywords
This article is cited by
-
Socio-cultural barriers to the delivery and utilisation of child healthcare services in rural Ghana: a qualitative study
BMC Health Services Research (2022)
-
A mixed-methods study exploring adherence to the referral of severely sick children in primary health care in Southern Ethiopia
Archives of Public Health (2021)
-
The added value of a mobile application of Community Case Management on referral, re-consultation and hospitalization rates of children aged under 5 years in two districts in Northern Malawi: study protocol for a pragmatic, stepped-wedge cluster-randomized controlled trial
Trials (2017)
-
Methodology for a mixed-methods multi-country study to assess recognition of and response to maternal and newborn illness
Journal of Health, Population and Nutrition (2017)
-
Leveraging the private sector for child health: a qualitative examination of caregiver and provider perspectives on private sector care for childhood pneumonia in Uttar Pradesh, India
BMC Health Services Research (2017)