Abstract
Background/Objectives:
Most insulin-requiring diabetes patients in Ethiopia have an atypical form of the disease, which resembles previous descriptions of malnutrition-related diabetes. As so little is known about its aetiology, we have carried out a case–control study to evaluate its social and nutritional determinants.
Subjects/Methods:
Men and women with insulin-requiring diabetes (n=107), aged 18–40 years, were recruited in two centres, Gondar and Jimma, 750 km northwest and 330 km southwest of the capital, Addis Ababa, respectively. Controls of similar age and sex (n=110) were recruited from patients attending other hospital clinics.
Results:
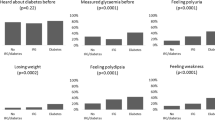
Diabetes was strongly associated with subsistence farming, odds ratio=3.5 (95% confidence interval: 1.5–7.8) and illiteracy/low levels of education, odds ratio=4.0 (2.0–8.0). Diabetes was also linked with a history of childhood malnutrition, odds ratio=5.5 (1.0–29.0) the mother's death during childhood, odds ratio=3.9 (1.0–14.8), and markers of poverty including poorer access to sanitation (P=0.004), clean water (P=0.009), greater overcrowding (P=0.04), increased distance from the clinic (P=0.01) and having fewer possessions (P=0.01). Compared with controls, people with diabetes had low mid upper arm circumference, body mass index (BMI) and fat/lean body mass (P<0.01). In addition, men with the disease tended to be shorter, were lighter (P=0.001), with reduced sitting height (P=0.015) and reduced biacromial (P=0.003) and bitrochanteric (P=0.008) diameters.
Conclusions:
Insulin-requiring diabetes in Ethiopia is strongly linked with poor education and markers of poverty. Men with the disease have associated disproportionate skeletal growth. These findings point towards a nutritional aetiology for this condition although the nature of the nutritional deficiency and its timing during growth and development remains obscure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abdulkadir J, Mengesha B, Gebriel ZW, Gebre P, Beastall G, Thompson JA (1987). Insulin-dependent ketosis-resistant diabetes in Ethiopia. Trans R Soc Trop Med Hyg 81, 539–543.
Abu-Bakare A, Taylor R, Gill GV, Alberti KG (1986). Tropical or malnutrition-related diabetes: a real syndrome? Lancet 1, 1135–1138.
Alemu S, Dessie A, Seid E, Bard E, Lee PT, Trimble ER et al. (2009). Insulin-requiring diabetes in rural Ethiopia: should we reopen the case for malnutrition-related diabetes? Diabetologia 52, 1842–1845.
Belcher DW (1970). Diabetes mellitus in northern Ethiopia. Ethiop Med J 8, 73–84.
Blom L, Persson LA, Dahlquist G (1992). A high linear growth is associated with an increased risk of childhood diabetes mellitus. Diabetologia 35, 528–583.
Bogin B, Varela-Silva MI (2008). Fatness biases the use of estimated leg length as an epidemiological marker for adults in the NHANES III sample. Int J Epidemiol 37, 201–209.
Desai M, Crowther NJ, Ozanne SE, Lucas A, Hales CN (1995). Adult glucose and lipid metabolism may be programmed during fetal life. Biochem Soc Trans 23, 331–335.
Durnin JV, Womersley J (1974). Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr 32, 77–97.
Elia M, Betts P, Jackson DM, Mulligan J (2007). Fetal programming of body dimensions and percentage body fat measured in prepubertal children with a 4-component model of body composition, dual-energy X-ray absorptiometry, deuterium dilution, densitometry, and skinfold thicknesses. Am J Clin Nutr 86, 618–624.
Gale EA, Gillespie KM (2001). Diabetes and gender. Diabetologia 44, 3–15.
Gatford KL, Mohammad SN, Harland ML, De Blasio MJ, Fowden AL, Robinson JS et al. (2008). Impaired beta-cell function and inadequate compensatory increases in beta-cell mass after intrauterine growth restriction in sheep. Endocrinology 149, 5118–5127.
Gill GV, Mbanya JC, Ramaiya KL, Tesfaye S (2009). A sub-Saharan African perspective of diabetes. Diabetologia 52, 8–16.
Gunnell DJ, Smith GD, Frankel SJ, Kemp M, Peters TJ (1998). Socio-economic and dietary influences on leg length and trunk length in childhood: a reanalysis of the Carnegie (Boyd Orr) survey of diet and health in prewar Britain (1937–39). Paediatr Perinat Epidemiol 12 (Suppl 1), 96–113.
Habtu E, Gill G, Tesfaye S (1999). Characteristics of insulin requiring diabetes in rural northern Ethiopia-a possible link with malnutrition? Ethiop Med J 37, 263–267.
Hay Jr WW (2006). Recent observations on the regulation of fetal metabolism by glucose. J Physiol 572, 17–24.
Hugh-Jones P (1955). Diabetes in Jamaica. Lancet 269, 891–897.
Kalk WJ, Huddle KR, Raal FJ (1993). The age of onset and sex distribution of insulin-dependent diabetes mellitus in Africans in South Africa. Postgrad Med J 69, 552–556.
Kensara OA, Wootton SA, Phillips DI, Patel M, Jackson AA, Elia M, Hertfordshire Study Group (2005). Fetal programming of body composition: relation between birth weight and body composition measured with dual-energy X-ray absorptiometry and anthropometric methods in older Englishmen. Am J Clin Nutr 82, 980–987.
Kotler DP, Burastero S, Wang J, Pierson Jr RN (1996). Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease. Am J Clin Nutr 64, 489S–497S.
LaPorte R, Matsushima M, Chang Y-F (1995). Prevalence and incidence of insulin-dependent diabetes. In: Harris MI, Cowie CC, Stern MP, Boyko EJ, Reiber GE, Bennett PH (eds). Diabetes in America (National Diabetes Data Group). NIH: Bethesda, MD. pp 37–46.
Levitt NS (2008). Diabetes in Africa: epidemiology, management and healthcare challenges. Heart 94, 1376–1382.
Li L, Dangour AD, Power C (2007). Early life influences on adult leg and trunk length in the 1958 British birth cohort. Am J Hum Biol 19, 836–843.
Lutale J, Thordarson H, Holm P, Eide G, Vetvik K (2007). Islet cell autoantibodies in African patients with Type 1 and Type 2 diabetes in Dar es Salaam Tanzania: a cross sectional study. J Autoimmune Dis 4, 4.
McLarty DG, Athaide I, Bottazzo GF, Swai AM, Alberti KG (1990). Islet cell antibodies are not specifically associated with insulin-dependent diabetes in Tanzanian Africans. Diabetes Res Clin Pract 9, 219–224.
Peters WH, Lester FT, Kohnert KD, Hildmann W (1986). The frequency of islet cell surface antibodies in newly diagnosed diabetics from Ethiopia. Exp Clin Endocrinol 87, 326–332.
Rao RH (1984). The role of undernutrition in the pathogenesis of diabetes mellitus. Diabetes Care 7, 595–601.
Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A (2003). Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease? Am J Clin Nutr 77, 726–730.
Sayer AA, Syddall HE, Dennison EM, Gilbody HJ, Duggleby SL, Cooper C et al. (2004). Birth weight, weight at 1 y of age, and body composition in older men: findings from the Hertfordshire Cohort Study. Am J Clin Nutr 80, 199–203.
Tripathy BB, Samal KC (1997). Overview and consensus statement on diabetes in tropical areas. Diabetes Metab Rev 13, 63–76.
Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R (2010). Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 125, 325–390.
Wadsworth ME, Hardy RJ, Paul AA, Marshall SF, Cole TJ (2002). Leg and trunk length at 43 years in relation to childhood health, diet and family circumstances; evidence from the 1946 national birth cohort. Int J Epidemiol 31, 383–390.
WHO (1999). Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. WHO: Geneva.
Zillikens MC, Conway JM (1990). Anthropometry in blacks: applicability of generalized skinfold equations and differences in fat patterning between blacks and whites. Am J Clin Nutr 52, 45–51.
Acknowledgements
We are grateful to Professor Tefera Belachew, Professor Henry Kahn and Professor Clive Osmond for advice. The study was supported by a grant from the Association of Physicians of Great Britain and Ireland in a programme funded through THET, London.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fekadu, S., Yigzaw, M., Alemu, S. et al. Insulin-requiring diabetes in Ethiopia: associations with poverty, early undernutrition and anthropometric disproportion. Eur J Clin Nutr 64, 1192–1198 (2010). https://doi.org/10.1038/ejcn.2010.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2010.143
Keywords
This article is cited by
-
Impact of prenatal famine exposure on adulthood fasting blood glucose level
Scientific Reports (2022)
-
Type 1 diabetes in Africa: an immunogenetic study in the Amhara of North-West Ethiopia
Diabetologia (2020)
-
Understanding the manifestation of diabetes in sub Saharan Africa to inform therapeutic approaches and preventive strategies: a narrative review
Clinical Diabetes and Endocrinology (2019)
-
Type 1 Diabetes in a Resource-Poor Setting: Malnutrition Related, Malnutrition Modified, or Just Diabetes?
Current Diabetes Reports (2018)
-
Dysglycemia associations with adipose tissue among HIV-infected patients after 2 years of antiretroviral therapy in Mwanza: a follow-up cross-sectional study
BMC Infectious Diseases (2017)