Abstract
Background:
The conduct of clinical trials should be an integral part of routine patient care. Treating patients in trials incurs additional costs over and above standard of care (SOC), but the extent of the cost burden is not known. We undertook a retrospective cost attribution analysis to quantitate the treatment costs associated with cancer clinical trial protocols conducted over a 2 year period.
Methods:
All patients entered into oncology (non-haematology) clinical trials involving investigational medicinal products in 2009 and 2010 in a single UK institution were identified. The trial protocols on which they were treated were analysed to identify the treatment costs for the experimental arm(s) of the trial and the equivalent SOC had the patient not been entered in the trial. The treatment cost difference was calculated by subtracting the experimental treatment cost from SOC cost. For randomised trials, an average treatment cost was estimated by taking into account the number of arms and randomisation ratio. An estimate of the annual treatment costs was calculated.
Results:
A total of 357 adult oncology patients were treated on 53 different trial protocols: 40 phase III, 2 randomised II/III and 11 phase II design. A total of 27 trials were academic, non-commercial sponsored trials and 26 were commercial sponsored trials. When compared with SOC, the average treatment cost per patient was an excess of £431 for a non-commercial trial (range £6393 excess to £6005 saving) and a saving of £9294 for a commercial trial (range £0 to £71 480). There was an overall treatment cost saving of £388 719 in 2009 and £496 556 in 2010, largely attributable to pharmaceutical company provision of free drug supplies.
Conclusion:
On an average, non-commercial trial protocols were associated with a small per patient excess treatment cost, whereas commercial trials were associated with a substantially higher cost saving. Taking into account the total number of patients recruited annually, treatment of patients on clinical trial protocols was associated with considerable cost savings across both the non-commercial and commercial portfolio.
Similar content being viewed by others
Main
The drug development process is well established and randomised clinical trials remain the gold standard for testing new treatments against standard of care in order to advance clinical practice (Vogelzang et al, 2012). Even so, the proportion of patients entering clinical trials worldwide is remarkably low. Since 2001, when under 4% of cancer patients took part in a clinical trial, recruitment increased six-fold over the following 10 years in the UK due to significant investment in a unique national research infrastructure (Department of Health, 2006; NCRN, 2011), whereas recruitment in the USA has remained static (Califf et al, 2012).
It is undisputed that conducting research incurs additional costs over and above standard of care (Emanuel et al, 2003), yet there is an international commitment to research being a core health service function (Zerhouni, 2003; Califf et al, 2012; The NHS Constitution, 2013). Attribution of research costs is complex and recovery of those costs, particularly for non-commercial clinical trials is very challenging (Snowdon et al, 2006; Seow et al, 2012). Costs incurred by conducting a clinical trial can broadly be attributed to one of the three elements (Attributing the costs of health and social care Research & Development (AcoRD), 2012): (1) research costs, that is, the costs of the trial itself, which end when the research ends and relate to activities being undertaken to answer the research question; (2) treatment costs, that is, the patient care costs, which would continue to be incurred if the patient care intervention continued to be provided after the trial had stopped; and (3) service support costs, that is, the additional patient care costs associated with the research, which would end once the trial had stopped, even if the patient care involved continued to be provided.
For commercially sponsored trials, all three elements would normally be met by the sponsor. In the UK, pharmaceutical companies have, for many years, been able to access service support from the national health service by formal adoption into a national clinical trials portfolio. For non-commercial studies, research costs are generally met by grant funders. Service support costs are met from local R&D budgets (via comprehensive local research networks), whereas treatment costs are met through the normal commissioning process. The latter has been the cause of significant disharmony between commissioners and providers of health care. In the USA, private insurance companies are not obliged to cover non-routine patient care costs (Anonymous, 2007). Cancer drugs are generally expensive and it is widely perceived that cancer clinical trials generate an excess treatment cost, despite a lack of evidence to support this view. A single retrospective review of 932 cancer patients recruited to 35 trials in the USA between 1998–1999 suggested that the incremental costs of direct care in clinical trials was 6.5% higher than what they would be outside of a trial (Goldman et al, 2003). The investigators concluded that the additional treatment costs of an open reimbursement policy for government-sponsored cancer clinical trials seem minimal. Even so, risk of excess treatment costs remains a barrier to academic clinical trials being performed in many countries today. We undertook a review of cancer clinical trials conducted in a single, research-active institution in the UK over a 2-year period (2009–2010), to identify the extent of treatment costs involved.
Materials and methods
Cambridge University Hospitals NHS Foundation Trust (Addenbrooke’s Hospital, Cambridge) is a major university teaching hospital and cancer centre in the UK. It also hosts the West Anglia Cancer Research Network (WACRN), one of the highest recruiting regional research networks in the UK, where 45.1% of patients newly diagnosed with cancer entered a research study in 2011/12. Although WACRN supports research across seven hospitals in the region, 64% of all patients were recruited at Addenbrooke’s hospital.
For this retrospective cost attribution analysis, all patients recruited to interventional, research ethics committee approved, oncology drug trials between 1 January 2009 and 31 December 2010 at Addenbrooke’s Hospital were identified from the Cambridge Cancer Trials Centre patient database. Haematology trials were excluded. The clinical trial protocols for each identified patient were reviewed to determine the treatment costs associated with each arm of the trial. The following activities were attributed to being treatment costs (as described in the AcoRD guidance): (1) supplying an investigation medicinal product and pharmacy costs associated with administering oral agents under investigation; (2) supplying and administering any active comparators, but not placebo; (3) nursing time to administer the drug, time taken to deliver the treatment either as an outpatient (‘day unit chair time’) or as an inpatient (‘bed days’); (4) investigations, including imaging and laboratory tests, which would continue to be incurred if the patient care service in question continued to be provided after the trial stopped; (5) additional clinic visits. Costs were calculated for the active treatment phase of the trial only and did not include follow-up once treatment had finished.
For all protocols, a standard of care (SOC) was identified as the standard treatment that would have been offered locally to the patient had the trial not been available. For randomised trials, if the control arm differed to the local standard treatment, the local standard treatment was used to cost SOC. The treatment costs of the SOC were determined as for the experimental arm.
Costs were determined for the duration of treatment defined in each trial protocol and did not include costs of follow-up once treatment stopped. For adjuvant, neo-adjuvant and some palliative protocols which specified the treatment programme duration, costs were determined for the entire prespecified treatment programme. For palliative protocols where treatment duration was until disease progression, the actual number of cycles and/or months of treatment delivered to the patients recruited to each protocol was obtained from the patient records and an average treatment duration was determined for each protocol. The same treatment duration was used for estimating SOC costs, unless the SOC treatment maximum duration was specified, in which case the shorter duration was used.
Cancer drug costs were obtained from the British National Formulary (2010) and excluded additional taxes or local negotiated discounts. Supportive drugs such as antiemetics, antidiarrhoeals, steroids, intravenous hydration fluids were excluded. For dose calculations, an average body surface area of 1.75 m2 was used. Staff and facility direct costs without overheads were obtained from local reference costs. Imaging and laboratory tests were costed locally or using the NIHR costing template. Where costs differed, local costs were used. The data was cross-checked with the lead clinical trials nurse responsible for each protocol.
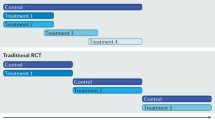
For each protocol, the treatment cost (TC) difference for the experimental arm(s) was the difference between the experimental arm treatment cost and the SOC cost. For randomised trials, an average treatment cost was attributed to the protocol, by taking into account the number of arms of the trial and randomisation ratio (see Table 1 as an example of how the TC difference was calculated).
Finally, using the total number of patients recruited to each trial protocol, the annual overall TC excess or saving in 2009 and 2010 was estimated.
Results
During the 2-year review period, 357 cancer patients were recruited to 53 different interventional clinical trials involving IMPs (Tables 2 and 3): 159 patients in 2009 and 198 patients in 2010. A total of 27 trials were academic, non-commercial sponsored trials with variable levels of industry support. A total of 26 trials were commercial sponsored trials, of which 26 of the non-commercial trials and 9 of the commercial trials were adopted in the NIHR portfolio. Thirty-nine of the 53 trials were randomised phase III design. The remainder were 1 non-randomised phase III, 2 randomised phase II/III, 9 randomised phase II and 2 non-randomised phase II trials. Patients received IMPs that were either unlicensed (22), licensed for the indicated disease (10) or licensed drugs being used in an unlicensed condition (21). Compared with 2009, in 2010, 24 new trials had opened to recruitment and 12 had closed.
The average TC per protocol across the portfolio of 53 trials ranged from an excess of £6393 to a saving of £71 480 (Figure 1). For 27 non-commercial trials (Table 2), the average TC per protocol ranged from an excess of £6393 to a saving of £6005 (mean excess TC was £431, median £126 per protocol). The main source of excess TC was due to extra hospital day unit delivery time associated with 9 protocols evaluating IMPs given in addition to, or in place of, SOC (7 protocols) or where the SOC was observation (2 protocols). For example, in the AVAST-M clinical trial comparing 12 months of 3 weekly adjuvant bevacizumab as treatment for patients with resected melanoma versus standard observation, the additional cost of treatment delivery accounted for £4250 (83%) of the £5144 excess TC. In this case, the investigation medicinal product cost did not contribute to the excess TC, as all bevacizumab was supplied free of charge by the manufacturer.
A total of 7 non-commercial trials were associated with a TC saving. Two of these trials, SCOT (comparing 3 months versus 6 months standard adjuvant chemotherapy in colorectal cancer) and PERSEPHONE (comparing 6 months versus 12 months standard adjuvant chemotherapy in breast cancer), were evaluating whether shorter durations of adjuvant treatment were as effective as SOC, in which the TCs were, in effect, halved. In 2 trials, the source of saving was free drug supplies in the experimental arms from manufacturers (SoFEA and BR13). As each trial randomised one or more treatment against a standard treatment, taking into account the number of arms and randomisation ratio, the average cost of a patient recruited to the protocol was less than SOC. In one trial (REAL-3), an industry grant provided a per payment fee of £1000 and in another trial (Telovac), one of the experimental arms was associated with fewer cycles of SOC chemotherapy given in association with the investigation medicinal product. In one trial (QUASAR2) comparing adjuvant capecitabine with capecitabine plus bevacizumab, the manufacturer supplied both the investigation medicinal product (bevacizumab) and the SOC (capecitabine) free of charge for patients recruited to either arm of the trial.
With the exception of REAL-3, treatment of patients on the other six non-commercial trial protocols associated with an overall TC saving offered financial benefits that would have been passed on to commissioners, primarily by the provision of free drug that would have had to be paid for if the patient was not on trial.
Considering the actual numbers of patients recruited to all of the non-commercial trials annually, the net TC saving was estimated at £67 962 in 2009 and £29 002 in 2010.
For the 26 commercial trials (Table 3), the average TC per protocol ranged from £0 to a saving of £71 480 (mean saving was £9294, median £4370 per protocol). Commercial trials were not associated with excess TCs, as income from the trial conduct was gained to cover all costs associated with treatment. The main source of cost saving was through provision of free drug supplies from the sponsor. In two renal cancer trials (Bevlin and Rad001), the sponsors provided the experimental drug free and in a third renal trial (Torisel404) both experimental and SOC drug were provided. With the exception of four randomised trials where SOC was observation or best supportive care, treating patients on the remaining 22 protocols would have passed on significant drug cost savings to commissioners, by avoiding the SOC costs the commissioners would have incurred if the patients were not on trial.
Using the actual numbers of patients recruited to all of the commercial trials, there was an estimated net treatment cost saving of £320 758 in 2009 and £467 554 in 2010.
Figure 2 summarises the distribution of average TCs for all 26 non-commercial and 27 commercial trial protocols. In general, it can be seen that both commercial and non-commercial trials saved drug costs, whereas the extent of drug and dispensing cost savings was markedly higher for commercial compared with non-commercial trials. The main source of excess TC was the cost of delivering treatment, most often generated by trials evaluating IMPs given in addition to SOC. The contribution of extra clinic visits and investigations, in particular CT scans used for response assessment, was significantly higher for commercial compared with non-commercial trials.
By taking into account the number of patients entered on each protocol, the overall annual TCs incurred were estimated. On an average, treating a patient on a clinical trial protocol was associated with a TC saving of £4340. The overall TCs incurred annually was a saving of £388 719 in 2009 and £496 556 in 2010 (Figure 3), around 90% of the savings coming from commercial sponsored trials.
Discussion
Research is considered an integral part of healthcare by many nations, as the benefits of new treatments tested in clinical trials are recognised to improve patient outcomes. It is important that the cost of that research is identified and properly funded. In the UK, the AcoRD guidance (2012) provides a framework to identify, attribute and recover the various costs associated with research, in a transparent, robust and consistent manner. It clarifies the distinction between research costs, service support costs and TCs. We have focused on quantitating the TCs associated with treating patients in cancer clinical trials, as uncertainty surrounding the size of cost difference between treatment in or outside of trials, particularly non-commercial trials, is a barrier to their efficient conduct.
We have previously sought to estimate the cost of the treatment administered to patients recruited to cancer trials using individual patient data from clinical research forms and pharmacy prescriptions (Corrie et al, 2011). However, TCs extend beyond the drug costs alone. So, to better inform service delivery, we developed a methodology designed to include all elements of TCs as described in the AcoRD guidelines. The method provides a unit TC difference associated with an individual trial protocol, taking into account the number of arms in a trial and, where appropriate, the randomisation ratio. The unit TC difference can only be an estimate, as the duration of treatment may vary for an individual patient, whereas for randomised trials, one might expect the estimate to be more accurate the more patients recruited to any protocol. In addition, we tailored SOC to local treatment guidelines, which may differ between regions. There are several limitations associated with this methodology. First, we did not take into account changes to the treatment plan associated with adverse drug reactions and did not include any associated non-elective hospital admissions, as individual patient data was not analysed in depth other than to estimate duration of palliative treatment in some instances. In addition, we did not include follow-up of patients after completion of anticancer therapy, assuming that this would account for a proportionally small element of treatment costs: commercial trials would be expected to fully reimburse all costs above SOC, whereas in general, frequency of follow-up in non-commercial trials tends to reflect routine follow-up arrangements. Finally, costing of commercial trials was based on direct costs only and did not include overheads charged to industry. Despite these limitations, we believe this methodology has the potential to be applied on a wider scale to inform providers and commissioners regarding the impact of conducting cancer clinical trials on health service resources.
Review of patients recruited to interventional cancer trials in a single research active institution over a 2-year period identified significant variation in associated TCs between protocols. The average TC for 27 non-commercial trials was an excess of £431 (range £6393 excess to £6005 saving) and for 26 commercial trials was an average saving of £9294 (range £0 to £71 480). Breaking down the TCs by the main categories, by far the largest contribution to cost savings was provision or reimbursement of IMPs by pharmaceutical companies, primarily as part of the conduct of commercial sponsored studies, but also, and to a lesser extent, in partnership with academic groups conducting non-commercial NIHR portfolio studies. The distribution of TCs was rather different for commercial and non-commercial trials. For non-commercial trials, the main excess TC was due to administering IMPs. For commercial trials, considerable extra costs were incurred by additional clinic visits and imaging investigations. This might suggest that pharmaceutical companies drive a more intensive patient management plan, and/or that, as many of the commercial protocols were for international multi-centre trials, they were designed to reflect practice in countries outside of the UK. Even so, because commercial trials were fully funded, the potential excess TCs associated with these protocols should not be passed on to commissioners. Our findings confirmed that the pathway for patients entered into academic trials did, in general, reflect routine clinical practice.
By assigning the 357 patients to the protocols in which they were enroled, the overall treatment cost saving to the NHS was estimated to be approaching £0.5 million per annum. In our view, this data provides overwhelming evidence to refute any concern that clinical research generates a cost pressure for the health service. On the contrary, we have demonstrated significant financial gains. The largest gains were from commercial sponsored trials. There is currently a growing emphasis on expanding the commercial trial portfolio across all disease areas. Although this may bring financial benefits, the main reason for our undertaking this review was to address concerns that academic clinical trials were a financial liability. Taken individually, this may be the case in some instances, but viewed across a whole portfolio, there are clear gains even for non-commercial clinical trials. Academic trials represent an important part of the NIHR portfolio, affording the opportunity to address questions that would not be a priority for industry sponsors. For example, two non-commercial trials testing whether shorter durations of adjuvant therapy might be as effective as longer durations were associated with significant TC savings during their conduct, whereas positive outcomes would have much wider implications for health service savings.
In summary, this unique analysis of TCs associated with patients recruited to cancer clinical trials indicates a wide range of per patient TC differences associated with individual trials compared with SOC, whereas the risk of there being an excess TC (as opposed to a saving) primarily lies with non-commercial studies. However, over the course of a year, clinical trials—both commercial and non-commercial—offer an opportunity to realise considerable TC savings. These findings support the Department of Health’s directive for commissioning of clinical trials as an integral part of service delivery. A balanced portfolio of both commercial and non-commercial research should offer the greatest benefits to patients and the overall health economy.
Change history
15 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Anonymous (2007) Developing an investigator site budget for clinical trials. J Oncol Pract 3: 94–97.
Attributing the costs of health and social care Research & Development (AcoRD) Department of Health (2012).
Califf RM, Filerman GL, Murray RK, Rosenblatt M (2012) The clinical trials enterprise in the United States: a call for disruptive innovation. National Academy of Sciences discussion paper pp1-21.
Corrie P, Weaver J, Chhabra A, Kingshott V, Hayton K, Bailey S, Andersen E, Inman I, Harris R, Follows G, Harrison M, Eisen T (2011) Attribution of costs associated with cancer trials conducted at a single UK institution. NCRI 2011: #A109.
Department of Health (2006) Best Research for Best Health: A New National Health Research Strategy. The NHS contribution to health research in England. Department of Health.
Emanuel EJ, Schnipper LE, Kamin DY, Levinson J, Lichter AS (2003) The costs of conducting clinical research. J Clin Oncol 21: 4145–4150.
Goldman DP, Berry SH, McCabe MS, Kilgore ML, Potosky AL, Schoenbuam ML, Schonlau M, Weeks JC, Kaplan R, Escarce JJ (2003) Incremental treatment costs in National Cancer Institute-sponsored clinical trials. JAMA 289: 2970–2977.
NCRN (2011) Celebrating a decade of progress through partnership in cancer research. 2001–2011.. http://ncrndev.org.uk/downloads/MiscDocs/NCRI_NCRN_Decade_Web.pdf.
Seow H-Y, Whelan P, Levine MN, Cowan K, Lysakoswki B, Kowasleski B, Snider A, Xu RY, Arnold A (2012) Funding oncology clinical trials: are Cooperative Group trials sustainable? J Clin Oncol 30: 1456–1461.
Snowdon C, Elbourne DR, Garcia J, Campbell MK, Entwistle VA, Francis D, Grant AM, Knight RC, McDonald AM, Roberts I (2006) Financial considerations in the conduct of multi-centre controlled trials: evidence from a qualitative study. Trials 7: 1–18.
The NHS Constitution (2013) Department of Health, March.
Vogelzang NJ, Benowitz SI, Adams S, Aghajanian C, Chang SM, Dreyer JE, Janne PA, Ko AH, Masters GA, Odenike O, Patel JD, Roth BJ, Samlowski WE, Seidman AD, Tap WD, Temel JS, Von Roenn JH, Kris MG (2012) Clinical Cancer Advances 2011: Annual Report on Progress Against Cancer From the American Society of Clinical Oncology. J Clin Oncol 30: 88–109.
Zerhouni E (2003) The NIH Roadmap. Science 302: 63–72.
Acknowledgements
We are grateful to all the patients who took part in the clinical trials, the Cambridge Cancer Trials Centre staff who cross-checked the data, local investigators who provided advice on specific protocols and Cancer Research UK colleagues who helped develop the methodology described here.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Liniker, E., Harrison, M., Weaver, J. et al. Treatment costs associated with interventional cancer clinical trials conducted at a single UK institution over 2 years (2009–2010). Br J Cancer 109, 2051–2057 (2013). https://doi.org/10.1038/bjc.2013.495
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.495
Keywords
This article is cited by
-
Optimising oncology drug expenditure in Ireland
Irish Journal of Medical Science (1971 -) (2024)
-
The economic impact of compassionate use of medicines
BMC Health Services Research (2021)
-
Clinical trials and drug cost savings for Italian health service
BMC Health Services Research (2020)
-
The chick chorioallantoic membrane as an in vivo xenograft model for Burkitt lymphoma
BMC Cancer (2014)