Abstract
Background
In patients with chronic heart failure, depression is common and associated with poor quality of life, more frequent hospitalizations, and higher mortality. Spiritual well-being is an important, modifiable coping resource in patients with terminal cancer and is associated with less depression, but little is known about the role of spiritual well-being in patients with heart failure.
Objective
To identify the relationship between spiritual well-being and depression in patients with heart failure.
Design
Cross-sectional study.
Participants
Sixty patients aged 60 years or older with New York Heart Association class II–IV heart failure.
Measurements
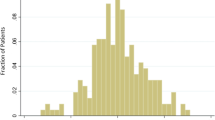
Spiritual well-being was measured using the total scale and 2 subscales (meaning/peace, faith) of the Functional Assessment of Chronic Illness Therapy—Spiritual Well-being scale, depression using the Geriatric Depression Scale—Short Form (GDS-SF).
Results
The median age of participants was 75 years. Nineteen participants (32%) had clinically significant depression (GDS-SF > 4). Greater spiritual well-being was strongly inversely correlated with depression (Spearman’s correlation −0.55, 95% confidence interval −0.70 to −0.35). In particular, greater meaning/peace was strongly associated with less depression (r = −.60, P < .0001), while faith was only modestly associated (r = −.38, P < .01). In a regression analysis accounting for gender, income, and other risk factors for depression (social support, physical symptoms, and health status), greater spiritual well-being continued to be significantly associated with less depression (P = .05). Between the 2 spiritual well-being subscales, only meaning/peace contributed significantly to this effect (P = .02) and accounted for 7% of the variance in depression.
Conclusions
Among outpatients with heart failure, greater spiritual well-being, particularly meaning/peace, was strongly associated with less depression. Enhancement of patients’ sense of spiritual well-being might reduce or prevent depression and thus improve quality of life and other outcomes in this population.



Similar content being viewed by others
References
Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65:119–128.
Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38:199–205.
Koenig HG. Depression in hospitalized older patients with congestive heart failure. Gen Hosp Psychiatry. 1998;20:29–43.
Sullivan MD, Newton K, Hecht J, Russo JE, Spertus JA. Depression and health status in elderly patients with heart failure: a 6-month prospective study in primary care. Am J Geriatr Cardiol. 2004;13:252–60.
Rumsfeld JS, Havranek E, Masoudi FA, et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42:1811–7.
Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–56.
Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med. 2002;162:1860–6.
McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361:1603–7.
Nelson CJ, Rosenfeld B, Breitbart W, Galietta M. Spirituality, religion, and depression in the terminally ill. Psychosomatics. 2002;43:213–20.
Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–92.
Jones AM, O’Connell JE, Gray CS. Living and dying with congestive heart failure: addressing the needs of older congestive heart failure patients. Age Ageing. 2003;32:566–8.
Westlake C, Dracup K. Role of spirituality in adjustment of patients with advanced heart failure. Prog Cardiovasc Nurs. 2001;16:119–25.
Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. 2004;44:2333–8.
Muldoon M, King N. Spirituality, health care, and bioethics. J Relig Health. 1995;34:329–49.
Sulmasy DP. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. 2002;42 Spec No 3:24–33.
Hauptman PJ, Havranek EP. Integrating palliative care into heart failure care. Arch Intern Med. 2005;165:374–8.
Pantilat SZ, Steimle AT. Palliative care for patients with heart failure. JAMA. 2004;291:2476–82.
Stevenson LW. Selection and management of candidates for heart transplantation. Curr Opin Cardiol. 1996;11:166–73.
Yesavage JA. Geriatric depression scale. Psychopharmacol Bull. 1988;24:709–11.
Yesavage JA, Sheikh JI. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;6:165–73.
Whooley MA, Browner WS. for the Study of Osteoporotic Fractures Research Group. Association between depressive symptoms and mortality in older women. Arch Intern Med. 1998;158:2129–35.
Arthur A, Jagger C, Lindesay J, Graham C, Clarke M. Using an annual over-75 health check to screen for depression: validation of the short Geriatric Depression Scale (GDS15) within general practice. Int J Geriatr Psychiatry. 1999;14(6):431–9.
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp). Ann Behav Med. 2002;24:49–58.
Bekelman DB, Sullivan M. Depression and anxiety in patients with chronic heart failure. In: Beattie J, Goodlin S, eds. Supportive Care of the Cardiac Patient. Oxford: Oxford University Press, In Press.
Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–55.
Spertus J, Peterson E, Conard MW, et al. Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J. 2005;150:707–15.
Heidenreich PA, Spertus JA, Jones PG, et al. Health status identifies heart failure outpatients at risk for hospitalization or death. J Am Coll Cardiol. 2006;47:752–6.
Mitchell PH, Powell L, Blumenthal J, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil. 2003;23:398–403.
Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–16.
Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The memorial symptom assessment scale short form (MSAS-SF). Cancer. 2000;89:1162–71.
Tranmer JE, Heyland D, Dudgeon D, Groll D, Squires-Graham M, Coulson K. Measuring the symptom experience of seriously ill cancer and noncancer hospitalized patients near the end of life with the memorial symptom assessment scale. J Pain Symptom Manage. 2003;25:420–9.
Brown RL, Leonard T, Saunders LA, Papasouliotis O. A two-item conjoint screen for alcohol and other drug problems. J Am Board Fam Pract. 2001;14:95–106.
Molloy DW, Standish TI. A guide to the standardized Mini-Mental State Examination. Int Psychogeriatr. 1997;9 (Suppl 1):87–94.
Geriatric Depression Scale. Available at: http://www.stanford.edu/~yesavage/GDS.html. Accessed October 10, 2006.
U.S. Census Bureau, Current Population Survey, 2006 Annual Social and Economic Supplement. Available at: http://pubdb3.census.gov/macro/032006/hhinc/new02_001.htm. Accessed October 10, 2006.
Beery TA, Baas LS, Fowler C, Allen G. Spirituality in persons with heart failure. J Holist Nurs. 2002;20:5–25.
Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliat Med. 2004;18:39–45.
Speck P, Higginson I, Addington-Hall J. Spiritual needs in health care. BMJ. 2004;329:123–4.
Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8:417–28.
Steinhauser KE, Voils CI, Clipp EC, Bosworth HB, Christakis NA, Tulsky JA. “Are you at peace?” One item to probe spiritual concerns at the end of life. Arch Intern Med. 2006;166:101–5.
Chochinov HM, Cann BJ. Interventions to enhance the spiritual aspects of dying. J Palliat Med. 2005;8(suppl 1):S103–15.
Levin JS. How religion influences morbidity and health: reflections on natural history, salutogenesis and host resistance. Soc Sci Med. 1996;43(5):849–64.
Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10:272–80.
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23:5520–5.
Mendes de Leon CF, Czajkowski SM, Freedland KE, Bang H, Powell LH, Wu C, et al. The effect of a psychosocial intervention and quality of life after acute myocardial infarction: the Enhancing Recovery in Coronary Heart Disease (ENRICHD) clinical trial. J Cardiopulm Rehabil. 2006;26:9–13.
Acknowledgements
The authors wish to thank the seriously ill patients in the study for their participation.
Potential Financial Conflicts of Interest
None disclosed
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented at the 52nd Annual Meeting of the Academy of Psychosomatic Medicine, November 17, 2005, Santa Ana Pueblo, NM; The Annual Assembly of the American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association, February 9, 2006, Nashville, TN; the 29th Society of General Internal Medicine Annual Meeting, April 26–29, 2006, Los Angeles, CA; and the 7th Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke, May 7–9, 2006, Washington, DC.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11606-007-0174-8
Rights and permissions
About this article
Cite this article
Bekelman, D.B., Dy, S.M., Becker, D.M. et al. Spiritual Well-Being and Depression in Patients with Heart Failure. J GEN INTERN MED 22, 470–477 (2007). https://doi.org/10.1007/s11606-006-0044-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-006-0044-9