Abstract
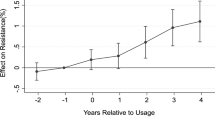
Because of evidence of causal association between antibiotic use and bacterial resistance, the implementation of national policies has emerged as a interesting tool for controlling and reversing bacterial resistance. The aim of this study was to assess the impact of public policies on antibiotic use in Europe using a differences-in-differences approach. Comparable data on systemic antibiotics administered in 21 European countries are available for a 11-year period between 1997 and 2007. Data on national campaigns are drawn from the public health literature. We estimate an econometric model of antibiotic consumption with country fixed effects and control for the main socioeconomic and epidemiological factors. Lagged values and the instrumental variables approach are applied to address endogeneity aspects of the prevalence of infections and the adoption of national campaigns. We find evidence that public campaigns significantly reduce the use of antimicrobials in the community by 1.3–5.6 defined daily doses per 1,000 inhabitants yearly. This represents an impact of roughly 6.5–28.3 % on the mean level of antibiotic use in Europe between 1997 and 2007. The effect is robust across different measurement methods. Further research is needed to investigate the effectiveness of policy interventions targeting different social groups such as general practitioners or patients.



Similar content being viewed by others
Notes
For more evidence on the impact of the French campaign to reduce inappropriate use of antibiotics, see also the recent study by Chahwakilian et al. [11], who analyse trends in antibiotic prescriptions between 1980 and 2009.
Antibiotic consumption data generally derive from reimbursement data or distribution/sales data, depending on the method for measuring antibiotic use employed by each national database. Assuming patient’s non-compliance to be a negligible factor implies that the quantity of antibiotics sold matches the quantity actually consumed. The latter is associated to antimicrobial resistance and represents the target of antibiotic policies.
Data are reliable and exhibit a good degree of comparability since the ESAC network screens for detection bias in sample and census data, bias by over-the counter sales and parallel trade, errors in assigning medicinal product packages to the Anatomical Therapeutic Chemical Classification (ATC), and errors in calculations of defined daily doses [20].
Public campaigns and policies are used interchangeably throughout the remaining of the paper. The reader should be aware that public campaigns represent a subset of possible antibiotic policies. The Netherlands, for instance, have strong antibiotic policies in place although the country did not conduct any public campaign during the study period.
In the literature, several approaches are discussed to estimate the causal impact of a “treatment variable” on an outcome variable, such as the DD estimator and the propensity score matching estimator. In this study, we use a differences-in-differences approach because of the relatively small panel data set with observations at the country level rather than at individual level. Using a propensity score matching approach requires, for instance, a large data set regarding the number of variables and the sample size. For a discussion on this issue, we refer the reader to studies by Frolich [21] and Heinrich et al. [22].
Initially, we also estimate Eq. (1) using ordinary least-squares (OLS) and random effects (RE) approaches.
As discussed by Bertrand et al. [14], conventional differences-in-differences standard errors may be biased because of serial correlation. A solution proposed by Arellano [28] is to compute cluster-robust standard errors. Kezdi [29] shows that cluster-robust estimates perform well in typical-sized panels, although they can be biased slightly downward if the number of countries is very small. In a Monte Carlo experiment, Kezdi [29] considers N = 10 to be a very small number of countries. In our case, N is equal to 20. Therefore, although the sample is relatively small, we believe that cluster-robust standard errors represent a viable solution to autocorrelation.
Although comparing antibiotic use among countries using DDD has a large consensus among researchers, one limitation is that this measure is not appropriate for all age groups. Indeed, using other measures may give different results, as illustrated by Goossens et al. [31].
Information on mortality for infectious diseases and price of pharmaceuticals are not available for all countries or years. This reduces the total number of observations in our final regressions.
It is important to underline that this variable is obtained from OECD data and is likely difficult to compare between countries. Mortality for infectious diseases is generally based on diagnostic discharge codes. Consequently, differences among countries may depend on different methods of determining this variable.
Preliminary OLS regressions show an R 2 adjusted of 0.59. The goodness-of-fit increases slightly with the inclusion of temporal dummy variables. The F test is 24.58 (12.51 with time dummies). This suggests that overall regressors has a significant impact on the dependent variable. Moreover, the mean variance inflation factor is lower than 3. Finally, the Shapiro-Wilk test as well as the Jarque-Bera test for normality of errors cannot be rejected using the conventional 95 % level of significance.
The results are confirmed if we include in the model the dummy variable POLICY 2 instead of POLICY 1. This takes a value equal to 1 in the years of campaign adoption as well as in the years post-campaign. The rationale of this indicator is that policies may take some time to show their effects or may have carryover effects. Although POLICY 1 seems to reflect more closely information collected in the review by Huttner et al. [12], POLICY 2 may provide a robustness check of our results based on POLICY 1. Since countries in the treatment group are assumed to implement policies for longer periods under POLICY 2 than under POLICY 1, the effect of policies could be biassed. We find that the estimated coefficients of POLICY 2 are slightly less significant than the coefficients of POLICY 1, which confirms the results and may suggest that policies have carryover effects beyond the year of policy implementation.
References
Park, S., Soumerai, S.B., Adams, A.S., Finkelstein, J.A., Jang, S., Ross-Degnan, D.: Antibiotic use following a Korean national policy to prohibit medication dispensing by physicians. Health Policy Plann. 20(5), 302–309 (2005)
Llor, C., Cots, J.M.: The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin. Infect. Dis. 48, 1345–1349 (2009)
Vaandnen, M.H., Pietila, K., Airaksinen, M.: Self-medication with antibiotics—does it really happen in Europe? Health Policy 77(2), 166–171 (2006)
Tan, L.J., Nielsen, N.H., Young, D.C., Trizna, Z.: Use of antimicrobial agents in consumer products. Arch. Dermatol. 138, 1082–1086 (2002)
Vande Sande-Bruinsma, N., Grundmann, H., Verloo, D., Tiemersma, E., Monen, J., Goossens, H., Ferech, M.: European antimicrobial resistance surveillance system, European surveillance of antimicrobial consumption project groups: antimicrobial drug use and resistance in Europe. Emerg. Infect. Dis. 14(11), 1722–1730 (2008)
Albrich, W.C., Monnet, D. L., Harbarth, S.: Antibiotic selection pressure and resistance in Streptococcus pneumoniae and Streptococcus pyogenes. Emerg. Infect. Dis. 10(3), 514–517 (2004)
Hawkings, N.J., Butler, C.C., Wood, F.: Antibiotics in the community: a typology of user behaviours. Patient Educ. Couns. 73, 146–152 (2008)
Sabuncu, E., David, J., Bernède-Baudin, C., Pèpin, S., Leroy, M., Boëlle, P.Y., Watier, L., Guillemot, D.: Significant reduction of antibiotic use in the community after a nationwide campaign in France, 2002–2007. PLoS Med. 6(6), 1–9 (2009)
Sabes-Figuera, R., Segú, J.L., Puig-Junoy, J., Torres, A.: Influence of bacterial resistances on the efficiency of antibiotic treatments for community-acquired pneumonia. Eur. J. Health Econ. 9(1), 23–32 (2008)
Goossens, H., Guillemot, D., Ferech, M., Schlemmer, B., Costers, M., van Breda, M., Baker, L.J., Cars, O., Davey, P.G.: National campaigns to improve antibiotic use. Eur. J. Clin. Pharmacol. 62, 373–379 (2006)
Chahwakilian, P., Huttner, B., Schlemmer, B., Harbarth, S.: Impact of the French campaign to reduce inappropriate ambulatory antibiotic use on the prescription and consultation rates for respiratory tract infections. J. Antimocrob. Chemother. 66, 2872–2879 (2011)
Huttner, B., Goossens, H., Verheij, T., Harbarth, S.: on behalf of the CHAMP consortium: Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatients in high-income countries. Lancet. Infect. Dis. 10, 17–31 (2010)
Masiero, G., Filippini, M., Ferech, M., Goossens, H.: Socioeconomic determinants of outpatient antibiotic use in Europe. Int. J. Public Health 55, 469–478 (2010)
Bertrand, M., Duflo, E., Mullainathan, S.: How much should we trust differences-in-differences estimates? Q. J. Econ. 119(1), 249–275 (2004)
Quick, J.D., Laing, R., Ross-Degnan, D.: Intervention research to promote clinically effective and economically efficient use of pharmaceuticals: the international network for rational use of drugs. J. Clin. Epidemiol. 44(II), 57S–65S (1991)
Rudholm, N.: Economic implications of antibiotic resistance in a global economy. J. Health Econ. 21, 1071–1083 (2002)
Coast, J., Smith, R., Millar, M.: An economic perpective on policy to reduce antimicrobial resistance. Social Sci. Med. 46, 29–38 (1998)
González Ortiz, L.G., Masiero, G.: Disentangling spillover effects of antibiotic consumption: a spatial panel approach. Appl. Econ. 45, 1041–1054 (2013)
Cizman, M., Beovic, B., Krcmery, V., Barsic, B., Tamm, E., Ludwig, E., Pelemis, M., Karovski, K., Grzesiowski, P., Gardovska, D., Volokha, A., Keuleyan, E., Stratchounski, L., Dumitru, C., Titov, L.P., Usonis, V., Dvorák, P.: Antibiotic policies in Central Eastern Europe. Int. J. Antimicrob. Agents 24(3), 199–204 (2004)
Vander Stichele, R., Elseviers, M., Ferech, M., Blot, S., Goossens, H.: European surveillance of antimicrobial consumption (ESAC): data collection performance and methodological approach. Br. J. Clin. Pharmacol. 58, 419–428 (2004)
Frolich, M.: Finite-sample properties of propensity-score matching and weighting estimators. Rev. Econ. Stat. 86(1), 77–90 (2004)
Heinrich, C., Maffioli, A., Vázquez, G.: A Primer for Applying Propensity-Score Matching. SPD Working papers 1005, Inter-American Development Bank, Office of Strategic Planning and Development Effectiveness (SPD), (2010)
Giavazzi, F., Tabellini, G.: Economic and political liberalizations. J. Monet. Econ. 52, 1297–1330 (2005)
Borg, M.A.: National cultural dimensions as drivers of inappropriate ambulatory care consumption of antibiotics in Europe and their relevance to awareness campaigns. J. Antimicrob. Chemother. 67(3), 763–767 (2012)
Deschepper, R., Grigoryan, L., Stålsby Lundborg, C., Hofstede, G., Cohen, J., Van der Kelen, G., Deliens, L., Haaijer-Ruskamp, F.M.: Are cultural dimensions relevant for explaining cross-national differences in antibiotic use in Europe? BMC Health Serv. Res. 8(123), (2008)
Harbarth, S., Albrich, W., Brun-Buisson, C.: Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg. Infect. Dis. 8(12), 1460–1467 (2002)
Swiss National Science Foundation: National Research Programme NRP 49 Antibiotic Resistance Final Report. http://www.nrp49.ch/upload/docs/Dokumente/NRP_49_Report_WEB%20mit%20Links.pdf. Accessed March 2012 (2007)
Arellano, M.: Computing robust standard errors for within-group estimators. Oxf. Bull. Econ. Stat. 49, 431–434 (1987)
Kezdi, G.: Robust standard error estimation in fixed-effects panel models. Hung. Stat. Rev. Spec. 9, 96-116 (2004)
WHO: ATC/DDD Index 2011. http://www.whocc.no/atc_ddd_index/. Accessed April 2011 (2011)
Goossens, H., Coenen, S., Costers, M., De Corte, S., De Sutter, A., Gordts, B., Laurier, L., Struelens, M.: Achievements of the Belgian antibiotic policy coordination committee (BAPCOC). Euro Surveill. 13(46), (2008)
OECD: OECD Health Data September 2010. http://www.oecd-ilibrary.org/statistics. Accessed April 2011 (2010)
Eurostat: Eurostat Statistics. http://epp.eurostat.ec.europa.eu/portal/page/portal/statistics/search_database. Accessed April 2011 (2010)
Cameron, A.C., Trivedi, P.K.: Microeconometrics. Cambridge University Press, New York (2005)
Molstad, S., Lundborg, C.S., Karlsson, A.K., Cars, O.: Antibiotic prescription rates vary markedly between 13 European countries. Scand. J. Infect. Dis. 34, 366–371 (2002)
Bjerrum, L., Sogaard, J., Hallas, J., Kragstrup, J.: Polypharmacy in general practice: differences between practitioners. Br. J. General Pract. 49(1), 95–98 (1999)
Cizman, M.: The use and resistance to antibiotics in the community. Int. J. Antimicrob. Agents 21, 297–307 (2003)
Das, J., Sohnesen, T.: Patient Satisfaction, Doctor Effort and Interview Location: Evidence from Paraguay. World bank policy research working paper 4086 (2006)
Baye, M.R., Maness, R., Wiggins, S.N.: Demand systems and the true subindex of the cost of living for pharmaceuticals. Appl. Econ. 29(9), 1179–1189 (1997)
Filippini, M., Masiero, G., Moschetti, K.: Small area variations and welfare loss in the use of outpatient antibiotics. Health Econ. Policy Law. 4, 55–77 (2009)
Filippini, M., Masiero, G., Moschetti, K.: Socioeconomic determinants of regional differences in outpatient antibiotic consumption: evidence from Switzerland. Health Policy. 78, 77–92 (2006)
Filippini, M., Masiero, G., Moschetti, K.: Regional consumption of antibiotics: a demand system approach. Econ. Model. 26, 1389–1397 (2009)
Di Matteo, L., Grootendorst, P.: Federal patent extension, provincial policies, and drug expenditures, 1975–2000. Can. Tax J. 50(6), 1913–1948 (2002)
Di Matteo, L.: The macro determinants of health expenditure in the United States and Canada: assessing the impact of income, age distribution and time. Health Policy. 71(1), 23–42 (2005)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filippini, M., Ortiz, L.G.G. & Masiero, G. Assessing the impact of national antibiotic campaigns in Europe. Eur J Health Econ 14, 587–599 (2013). https://doi.org/10.1007/s10198-012-0404-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-012-0404-9