Abstract
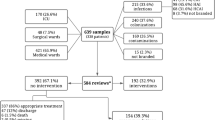
We evaluated the impact of a prospective audit and feedback antimicrobial stewardship program (ASP) on antibiotic prescription and resistance trends in a hematology-oncology unit in a university hospital (National University Cancer Institute, Singapore [NCIS]). A prospective interrupted time-series study comprising 11-month pre-intervention (PIP) and intervention evaluation phases (IEP) flanking a one-month implementation phase was carried out. Outcome measures included defined daily dose per 100 (DDD/100) inpatient-days of ASP-audited and all antibiotics (encompassing audited and non-audited antibiotics), and the incidence-density of antibiotic-resistant microorganisms at the NCIS. Internal and external controls were DDD/100 inpatient-days of paracetamol at the NCIS and DDD/100 inpatient-days of antibiotics prescribed in the rest of the hospital. There were 580 ASP recommendations from 1,276 audits, with a mean monthly compliance of 86.9%. Significant reversal of prescription trends towards reduced prescription of audited (coefficient = −2.621; 95% confidence interval [CI]: −4.923, −0.319; p = 0.026) and all evaluated antibiotics (coefficient = −4.069; 95% CI: −8.075, −0.063; p = 0.046) was observed. No changes were seen for both internal and external controls, except for the reversal of prescription trends for cephalosporins hospital-wide. Antimicrobial resistance did not change over the time period of the study. Adverse outcomes—the majority unavoidable—occurred following 5.5% of accepted ASP recommendations. Safe and effective ASPs can be implemented in the complex setting of hematology-oncology inpatients.



Similar content being viewed by others
References
Dellit TH, Owens RC, McGowan JE Jr et al (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177
Allerberger F, Mittermayer H (2008) Antimicrobial stewardship. Clin Microbiol Infect 14:197–199
Rolston KV (2009) The use of new and better antibiotics for bacterial infections in patients with leukemia. Clin Lymphoma Myeloma 9(Suppl 3):S357–S363
Metjian TA, Prasad PA, Kogon A et al (2008) Evaluation of an antimicrobial stewardship program at a pediatric teaching hospital. Pediatr Infect Dis J 27:106–111
Agwu AL, Lee CK, Jain SK et al (2008) A World Wide Web-based antimicrobial stewardship program improves efficiency, communication, and user satisfaction and reduces cost in a tertiary care pediatric medical center. Clin Infect Dis 47:747–753
Cheng VC, To KK, Li IW et al (2009) Antimicrobial stewardship program directed at broad-spectrum intravenous antibiotics prescription in a tertiary hospital. Eur J Clin Microbiol Infect Dis 28:1447–1456
Jin J, Lee YM, Ding Y et al (2010) Prospective audit of febrile neutropenia management at a tertiary university hospital in Singapore. Ann Acad Med Singapore 39:453–459
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2009. Available at: http://www.whocc.no/atcddd/. Last accessed 23rd February 2011
Clinical Laboratory Standards Institute (CLSI) (2005) Performance standards for antimicrobial susceptibility testing. Supplement M100-S14. CLSI, Wayne, PA, USA
Hsu LY, Tan TY, Jureen R et al (2007) Antimicrobial drug resistance in Singapore hospitals. Emerg Infect Dis 13:1944–1947
Fraser GL, Stogsdill P, Dickens JD Jr et al (1997) Antibiotic optimization. An evaluation of patient safety and economic outcomes. Arch Intern Med 157:1689–1694
Carling P, Fung T, Killion A et al (2003) Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol 24:699–706
Bantar C, Sartori B, Vesco E et al (2003) A hospitalwide intervention program to optimize the quality of antibiotic use: impact on prescribing practice, antibiotic consumption, cost savings, and bacterial resistance. Clin Infect Dis 37:180–186
Wong-Beringer A, Nguyen LH, Lee M et al (2009) An antimicrobial stewardship program with a focus on reducing fluoroquinolone overuse. Pharmacotherapy 29:736–743
Yong MK, Buising KL, Cheng AC et al (2010) Improved susceptibility of Gram-negative bacteria in an intensive care unit following implementation of a computerized antibiotic decision support system. J Antimicrob Chemother 65:1062–1069
Cook PP, Catrou PG, Christie JD et al (2004) Reduction in broad-spectrum antimicrobial use associated with no improvement in hospital antibiogram. J Antimicrob Chemother 53:853–859
Hsu LY, Tan TY, Tam VH et al (2010) Surveillance and correlation of antibiotic prescription and resistance of Gram-negative bacteria in Singaporean hospitals. Antimicrob Agents Chemother 54:1173–1178
Joshi VD, Lim JF (2010) Health insurance in Singapore: who’s not included and why? Singapore Med J 51:399–405
Owens RC Jr, Fraser GL, Stogsdill P, Society of Infectious Diseases Pharmacists (2004) Antimicrobial stewardship programs as a means to optimize antimicrobial use. Insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy 24:896–908
Acknowledgments
We would like to acknowledge Dr. Jennifer Ho, Dr. Eng-Kiang Lee, and Dr. Indumathi Venkatachalam for their assistance in running the antimicrobial stewardship program (ASP) and Mr. Wee Chuan Hing for his assistance with the data retrieval. We would also like to thank the clinical staff of the National University Cancer Institute, Singapore (NCIS) for their support of the program.
Conflicts of interest
This study was carried out as part of our routine work, and was unfunded.
L.-Y.H. has received research funding and speaker’s honoraria from Pfizer, AstraZeneca, Janssen & Cilag, and Merck, Sharpe & Dohme. All other authors declare no competing interests with regards to the published material in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yeo, CL., Chan, D.SG., Earnest, A. et al. Prospective audit and feedback on antibiotic prescription in an adult hematology-oncology unit in Singapore. Eur J Clin Microbiol Infect Dis 31, 583–590 (2012). https://doi.org/10.1007/s10096-011-1351-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1351-6